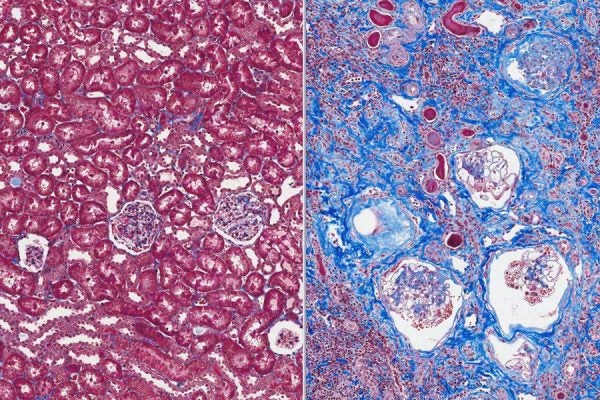
Fibrosis is normally beneficial, but excessive amounts can leave tissues stiff and undermine their function.
By Charlie Feigenoff. Originally published in UVA Today.)
Fibrosis is a deadly thread that winds its way through scores of fatal diseases, from pulmonary fibrosis and heart failure to chronic kidney disease and cirrhosis of the liver.
Under normal conditions, fibrosis is beneficial, the scaffolding of scar tissue the body erects to repair wounds. But when excessive or unchecked, fibrosis can riddle organs with stiff tissue, diminishing their flexibility and undermining their function. All told, fibrosis is implicated in or directly responsible for as much as 40 percent of all deaths worldwide.
“In many ways, fibrosis is as significant a problem as cancer, but we have no reliable approaches for early detection or effective treatment,” biomedical engineering professor Thomas Barker, an expert in pulmonary fibrosis, said. “In effect, we are where cancer researchers were in the 1980s.”
Positioning UVA as a Center for Fibrosis Research
The primary reason for this state of affairs: The process of fibrosis is itself exquisitely complicated. Added to that, the circumstances that can generate uncontrolled, indiscriminate fibrosis can vary significantly from organ to organ and from disease to disease.
To jump-start progress, Barker, working with colleagues in the University of Virginia schools of Engineering and Medicine, has launched the Fibrosis Initiative, an effort to mobilize UVA researchers conducting fibrosis-related studies and build connections among them that will lead to potentially groundbreaking, cross-disciplinary investigations.
“Our goal is to produce fundamental insights that can be applied across organ systems,” Barker said.
The Fibrosis Initiative will facilitate research funding, with the ultimate aim of securing a National Institutes of Health “Center of Excellence” award. If successful, Barker envisions UVA emerging as a critical node in the worldwide effort to diagnose and treat fibrosis.
The reception to Barker’s project has been enthusiastic. “I think this big-tent approach is exactly what we need, because fibrosis cuts across so many different areas,” said Dr. Mark Okusa, chief of the Division of Nephrology and an expert in acute kidney disease.
Associate professor Andrew Dudley, a tumor biologist who has an interest in the contribution of fibrosis to cancer-associated blood vessel formation, echoed Okusa’s thought. “Creating a network of people who are aware of what other people are doing is incredibly valuable,” he said. “I have already benefited at UVA from the exchange of ideas and access to guidance and resources. The Fibrosis Initiative will build on a solid foundation.”
Pamela M. Norris, UVA Engineering’s executive associate dean for research, said the UVA Fibrosis Initiative is another example of the University’s focus on engineering for medicine, with researchers bringing together the science, technology and practice of medical care to make powerful advances in treatments.
“UVA has a unique ability to do this because we are one of the few top research universities in the country with schools of engineering and medicine separated by less than a mile,” Norris said. “Approximately half of the faculty in our Biomedical Engineering Department are jointly appointed with our School of Medicine, and that’s a huge advantage for making discoveries about disease and precision treatments.”
Outsmarting Fibrosis
Barker’s work illustrates the challenges that researchers face. Among other grants, Barker holds a prestigious NIH Director’s Transformative Research Award for research on idiopathic pulmonary fibrosis, a deadly disease that affects as many as 500,000 Americans.

Thomas Barker, who is leading the Fibrosis Initiative, said, “We are where cancer researchers were in the 1980s.” (Photo by Tom Cogill)
When tissue is damaged, fibroblast cells migrate to the wound site, where a combination of mechanical and chemical changes in the microenvironment converts them to myofibroblasts, which in turn deposit the collagen that makes up the scaffolding, or extracellular matrix, that holds tissue together.
Idiopathic pulmonary fibrosis is characterized by runaway extracellular matrix assembly as increasing tissue stiffness drives the differentiation of additional myofibroblasts. Barker’s goal is to reconfigure the molecular mechanisms that enable cells to sense this stiffness, programming them to deliver fibrosis-reducing therapy instead of encouraging myofibroblastic differentiation.
This is just one approach that Barker is using to short-circuit fibrosis. This year, Barker and his colleagues have published a number of papers that point to a molecular switch that could be used to interrupt fibrosis. The extracellular matrix is not a passive structure, and changes in the components such as the protein fibronectin can alter the behavior of cells in their environment.
Barker’s group found that mechanical stresses on fibronectin can change the way it folds and, in the process, change a domain that binds cell surface molecules called integrins that influence fibrotic progression and blood vessel formation. This paper appeared in ACS Nano, a publication of the American Chemical Society.
In a related paper published in Nature Materials, Barker and his colleagues showed that changes in fibronectin folding that accommodated one subset of integrin rather than another would determine the quality of the blood vessels that result, including those that are found in tumors.
“The possibility that we can manipulate that integrin switch makes it a potential target for drug therapy,” Barker said.
Starting from a Position of Strength
UVA has several key advantages that make it an ideal home for the Fibrosis Initiative. First, it has assembled a diverse group of faculty with expertise in extracellular matrix biology. This includes a core group in the Department of Biomedical Engineering – among them professors Jeffrey Holmes and Shayn Peirce-Cottler as well as associate professor Jeffrey Saucerman – who focus on fundamental fibrotic processes. All three are combined faculty for the schools of Engineering and Medicine, and all secured major grants this year for ambitious fibrosis-related research.
In addition, UVA has a wealth of clinicians and scientists in fields like pulmonology, cardiology, nephrology, oncology and microbiology investigating fibrosis in the context of specific organ systems or diseases. In other words, it has already assembled the critical mass of fibrosis researchers needed to make progress.
UVA is also internationally known for its strengths in computational and quantitative biology. The ability to model complex systems at multiple scales is essential to rapid advances in the field.
“Fibrosis is a great example of a problem that is complicated enough that you need systems thinking and modeling in order to crack it,” Holmes said.
UVA also has exceptional depth and breadth in preclinical and clinical imaging methodologies. This includes such modalities as MRI, PET, ultrasound and such cutting-edge technologies as photo-acoustic imaging. For instance, thanks to the efforts of professor Frederick Epstein, chair of UVA’s Biomedical Engineering Department and professor of radiology, and cardiovascular imaging specialists Dr. Christopher Kramer and Dr. Michael Salerno, UVA is a leader in developing methods to quantitatively assess diffuse fibrosis in the heart, including the right ventricle, which can produce heart failure in people with pulmonary hypertension.
“These techniques are important because they will enable us to determine if therapies that reduce cardiac fibrosis are effective,” Epstein said.
Ultimately, it is the culture of collaboration at UVA that will be pivotal to the success of the Fibrosis Initiative. “Researchers here are truly open to helping other labs, even if there is no immediate benefit to themselves,” Saucerman said.
Dr. Alexander Krupnick, a thoracic surgeon investigating the role of fibrosis in lung transplant rejection, echoed this thought. “UVA has brought together a superb group of people who actively look for opportunities to combine forces,” he said. “This combination is very rare.”
Filed Under: Media Highlights, Research
Tags: biomedical engineering

Comments