Message from Mohan Nadkarni MD, Division Chief of General, Geriatric, and Palliative Medicine
 I am pleased to highlight exciting programs and faculty for our busy Division. We have a broad array of faculty, APPs, and staff whose clinical care, education, and scholarship span the breadth of all Internal Medicine. We see a large number and variety of patients on a longitudinal basis in various settings. Educationally, we are the backbone of GME and UME medical training, providing 3-year mentorship to our IM residents at University Medical Associates and University Physicians Charlottesville and vital training in Geriatrics and Palliative care. Many faculty also provide four-year mentoring to medical students via the FCM course. Our Palliative and Geriatric sections also host vibrant fellowship programs. We are enhancing our scholarship activities with new research directors for the Division. We highlight our retiring and new faculty members, introduce the new suboxone clinic at UMA, and describe Dr Bogg’s research work on Epic SIGNAL data analysis, the Geriatric Virginia at Home program, and the continued excellent palliative care programs. I am so thankful and impressed by the tremendous and varied care, education, and research our Division provides.
I am pleased to highlight exciting programs and faculty for our busy Division. We have a broad array of faculty, APPs, and staff whose clinical care, education, and scholarship span the breadth of all Internal Medicine. We see a large number and variety of patients on a longitudinal basis in various settings. Educationally, we are the backbone of GME and UME medical training, providing 3-year mentorship to our IM residents at University Medical Associates and University Physicians Charlottesville and vital training in Geriatrics and Palliative care. Many faculty also provide four-year mentoring to medical students via the FCM course. Our Palliative and Geriatric sections also host vibrant fellowship programs. We are enhancing our scholarship activities with new research directors for the Division. We highlight our retiring and new faculty members, introduce the new suboxone clinic at UMA, and describe Dr Bogg’s research work on Epic SIGNAL data analysis, the Geriatric Virginia at Home program, and the continued excellent palliative care programs. I am so thankful and impressed by the tremendous and varied care, education, and research our Division provides.
~Mohan Nadkarni MD
Education Updates
 Recent Advances In Clinical Medicine
Recent Advances In Clinical Medicine
by David Callender, MD
The Recent Advances in Clinical Medicine CME Conference, now in its 51st year, is a CME conference sponsored by the Department of Medicine. It focuses on recent developments and periodic medical topic updates relevant to generalists. It draws many attendees from across the Commonwealth, including MDs and APPs. The three-day conference will be held in downtown Omni in late October. The main sessions are organized by specialty/subspecialty or multidisciplinary theme. There are generally three talks for each session, each 25 minutes long, followed by a 20-minute Q&A for the three speakers. There are 37 speakers in total. We get about 200+ internists, family doctors, NPs, and PAs from around the state, region, and country.
The planning committee meets once in the winter (Jan/Feb) to review the prior meeting’s evaluations and discuss possible format changes and possible themes and specific topics to highlight for the coming year. Committee members recruit speakers from their respective divisions/departments by April. Planning committee members include Michael Ayers (Cards), Michael Keng (Heme/Oncology), Brian Wentworth (GI), Patrick Jackson (ID), Beth-Jaeger Landis (APP), Daphne Knicely (Nephrology), Donna Landen (FM), Kaitlin Love (Endocrine), Hannah Mannem (Pulmonary), Kathryn Reid (Nursing), and Andrew Whitman (Pharm).
 UMA Office-Based Opioid Treatment (OBOT) Program Provides Resident Training
UMA Office-Based Opioid Treatment (OBOT) Program Provides Resident Training
by Rachel Kon MD
As the opioid crisis continues, the last year has brought the end of X-waivers for prescribing Suboxone for opioid use disorder (OUD), increased substance use disorders (SUD) training requirements to get a DEA license, and continued high demand for OUD treatment services. Co-occurring chronic pain and OUD are common in our safety-net resident continuity clinic, which leads to frustration for both patient and provider when conflict occurs around pain management plans. If patients can be rotated to a safer partial agonist opioid by partnering with their trusted medical home, the doctor-patient relationship can flourish, and overdoses can be reduced.
Our IM residency program has responded to these changes by increasing the classroom training and creating more clinical experience for our IM residents with the goal that they graduate prepared to initiate and maintain patients on Suboxone for OUD treatment when they graduate. To provide clinical training and meet patient demand for low-barrier OUD treatment in the primary care setting, we have started an OUD treatment program within our University Medical Associates (UMA) resident continuity clinic called UMA OBOT. This program welcomes our current patients to a specialized session on Monday afternoons with trained faculty, pharmacists to counsel on films, a social worker to access counseling needs and give resources, and an RN coordinator.
Patients with OUD who are ready to start treatment but do not have a PCP can be referred to UMA OBOT as both an outpatient prescriber and a new PCP. Our PGY2 IM residents will rotate through this session several times to both experience initiating and titrating Suboxone for OUD and accruing 1-2 patients in OUD treatment for their continuity panel, so they gain experience in maintenance therapy.
Dr. Rachel Kon has spearheaded this initiative with funding from her UVA Health GME Master Educator award. Dr. Kon has been collaborating with Family Medicine PCC faculty and UVA Psychiatry OBOT providers to learn from their experience and develop a nested OUD treatment program in the primary care setting.
Dr. Alexandra Schwab was recruited to devote a year before fellowship training to getting the logistics of the UMA OBOT program off the ground and precept the session. Dr. Schwab is working 50% inpatient and 50% outpatient this year, positioning her to collaborate with clinicians in both settings to develop safe pathways to engage our patients in OUD treatment. Dr. Margaret Hayden is arriving in September to the UMA faculty from the University of Alabama with significant experience treating OUD in safety net clinics similar to UMA. She will facilitate key educational sessions for our residents. RN of the Year award winner by our residents, Missy Warren, has been recruited as our RN coordinator. Our current ambulatory chief resident, Dr. Thompson Barr, has led faculty development for our UMA firm attendings and assisted Dr. Kon with redesigning didactic sessions in the IM residency curriculum.
Once these initiatives are fully implemented, we expect all IM residents to graduate with both the classroom and clinical experience to meet the needs of our patients suffering from OUD. We hope that being able to offer OUD treatment will improve the meaning and satisfaction of residents providing primary care for patients with chronic pain.
Please send questions or patient referrals to Alexandra Schwab, Melissa Warren, and Rachel Kon by Epic staff message. We look forward to growing this program to meet UVA IM’s patient and educational needs.
 Using Epic Signal User Analytics To Give Feedback To Residents
Using Epic Signal User Analytics To Give Feedback To Residents
by Zachary Boggs, MD
Residents often say that their Epic Inbasket is one of the most significant contributors to burnout. We conducted a needs assessment survey among the internal medicine residents, and this was shown to be true. A recent survey of internal medicine program directors revealed substantial patient safety concerns with unsupervised residents inbasket decisions. Inter-visit care is very challenging for residents, and we have a limited ability to supervise this aspect of patient care. As clinic preceptors, we often have a hard time giving feedback to residents on their inbasket management because we have limited opportunity to observe how they provide inter-visit care. We developed a new curriculum to tackle these issues with inbasket management using Epic Signal.
Epic Signal is a program that provides access to user-level performance metrics. Signal has guided 1-on-1 training for physicians on their electronic health record processes to improve efficiency. User data has also been used to identify the risk of burnout using metrics such as “pajama time.” Trainee user data can be used similarly to help residency programs identify residents struggling with inter-visit care and offer personalized coaching. Epic Signal data offers excellent potential to help improve trainee digital competency through individualized training and may allow for increased trainee supervision.
We held training sessions for resident continuity clinic preceptors on interpreting Signal data, giving personalized feedback, and developing individualized improvement plans for residents. The training emphasized that data should be presented as formative information to identify growth areas to improve their quality of life and enhance patient safety. We focused on key objectives for our first iteration of this curriculum: how to use efficiency tools like QuickActions and ancillary support for patient messages.
Our clinic preceptors met with residents for their first feedback sessions using Signal data this Spring, and we plan to repeat the process every six months. We have heard that residents appreciate seeing their Signal data and have made informed improvements with inbasket management. The clinic preceptors have been enlightened by seeing their residents’ data and have appreciated enhanced oversight. We plan to study the effects of this curriculum on burnout using surveys.
In addition to individualized feedback meetings using Signal data, we offer additional training for residents using didactics and workshops, optional peer support, and an optional self-directed module. If you’d like to hear more about our curriculum or other ways we can use Epic Signal, please get in touch with Zachary Boggs at ZB3CA@uvahealth.org.
 Palliative Fellow Named Medical Director For Hospice Of The Piedmont
Palliative Fellow Named Medical Director For Hospice Of The Piedmont
by Leslie Blackhall, MD
In June, the UVA Palliative Medicine fellowship was proud to graduate two great physicians. Dr. Kell Mitchell will stay in Virginia to expand quality end-of-life care access as a Medical Director for Hospice of the Piedmont in the Culpeper region. With her added expertise from a palliative fellowship, Dr. Maki Nakazato returns to her home in California to provide quality geriatric care. Her expertise will undoubtedly be a valuable addition to UCSF’s outpatient Geriatric care services. The fellowship welcomes Alex Schofeit after he graduated from his Internal Medicine Residency at Cooper University in June.
Palliative Care Continues To Expand Services
byLeslie Blackhall, MD
The palliative care team continues providing comprehensive care to patients with a life-limiting illness. We have expanded our collaborative practice models with multiple services to improve patient care, including Hematology, Cardiology, and General Medicine. We are working with the UVA Health System, Hospice of the Piedmont, and Legacy Hospice to improve patients’ access to hospice services at the end of life, including streamlining inpatient hospice conversation and discharges to hospice for hospitalized patients, as well as those in ambulatory and ED settings. We worked with Pulmonary Medicine to recruit and hire Katie Waybill, MD, who completed pulmonary/critical care and palliative care fellowships. She will work part-time with our outpatient clinic to help expand services for patients with advanced pulmonary disease.
Clinical Updates
 SDCC (Same Day Care Clinic)
SDCC (Same Day Care Clinic)
by Sidhartha Pani, MD
I joined the University of Virginia in December 2023 as the Medical Director of the Same Day Care Clinic (SDCC). Formerly the COVID clinic, the SDCC opened in October 2023. Located on the first floor of 1222 JPA, it is easily accessible and located next to the Sleep Clinic.
The clinic has an excellent team of nurses, medical assistants, and front desk staff. There are six APP providers, of whom two primarily work virtually. The SDCC is open on weekdays from 8 AM to 5 PM. The clinic is designed to see follow-ups from the ED, minor acute issues, and same-day overflows from other outpatient clinics. The nurses regularly schedule infusions at the clinic (including remdesivir, IV antibiotics, iron infusions, and IV hydration). They also administer the rabies vaccine, perform wound care, and remove stitches.
Patients seeking virtual care can self-schedule through MyChart. Pods and doctor’s offices schedule onsite visits following communications between patients and their care providers via MyChart. While walk-ins are not encouraged, the SDCC accommodates occasional ones when possible.
The number of monthly visits at the SDCC has increased remarkably from just over 400 visits in October 2023 to almost double that by July 2024. In June 2024, we were declared the number two best-performing clinic based on patient access, patient experience, and financials.
We have come a long way and look forward to more innovations in the months ahead.
 Geriatrics Clinical Service Expansion
Geriatrics Clinical Service Expansion
by Justin Mutter, MD
The Section of Geriatrics continues to serve many communities through its JABA and Colonnades Clinics, the Westminster Canterbury Clinic and Medical Directorship, and the Virginia at Home program. We have just completed our first year of partnership providing a consultative clinic with the Veterans Affairs (VA) primary care clinic in Charlottesville. We are excited to welcome Dr. Benjamin Cahill to the faculty, whose clinical responsibilities will include leading the VA partnership. This fall, the Section will launch a new inpatient consultative collaboration with UVA Trauma Services. We are thrilled that new faculty member Dr. Matthew Van Dongen will lead this effort.
Geriatrics Matches Two Fellows
by Justin Mutter, MD
Educational Program Highlight: This summer, the Section welcomed two excellent new fellows in Geriatric Medicine, Dr. Michelle Lee and Dr. Louay Zumot. This year marks the second consecutive year that geriatrics faculty have filled both fellowship positions.
Research Updates
Endowed Geriatric Research Professorship Established
by Justin Mutter, MD
This summer, the UVA Board of Visitors approved a new endowed research professorship in the Section of Geriatrics, provided generously by a grateful patient. A nationwide search for this new faculty role will begin this fall.
Palliative Research Highlights
by Leslie Blackhall, MD
Current research projects include studies on the impact of early palliative care for patients with high-risk leukemia and NSC lung cancer. With Virginia LeBaron RN PhD from the SON, we are participating in a study on using smart health technology to monitor cancer pain and the use of opioids in the home setting and pain, and a pilot study of a novel mobile health device to improve provider-patient. David Ling MD is analyzing PRO data collected by our team from patients with advanced cancer to look at the ways changes in symptoms such as pain, fatigue, and functional status correlate with changes in quality of life as patients approach the end of life.
 Newly Named Co-Directors Of Division Research and Scholarship
Newly Named Co-Directors Of Division Research and Scholarship
by Milad Memari, MD
We are thrilled to introduce ourselves in our new roles in the Division as the Director of Medical Education Research and Scholarship (Dr. Milad Memari GPY7RB@uvahealth.org ) and Director of Clinical Research and Scholarship (Dr. Tabor Flickinger TES3J@uvahealth.org ). We aim to advance the scholarly mission of the Division, including increasing faculty engagement in research, providing faculty development and resources to support academic work, and providing a forum for collaboration and advancement of scholarly endeavors. We greatly appreciate the responses we received on our recent faculty survey to inform our efforts. Our planned next steps include regular division research meetings (more to come soon!), works-in-progress meetings and writing groups, faculty development sessions, and national meeting scholarly submission preparation/planning. We look forward to inviting outside speakers with expertise in educational and clinical research and scholarship to interact with our group. Ultimately, our goal is to support the faculty and grow the scholarly endeavors of our Division, and we are excited to engage with you all on this moving forward!
Dr. Flickinger’s research focuses on quality improvement, health equity, and patient-clinician communication. She is a co-investigator on the PositiveLinks (PL) project, funded by the Virginia Department of Health (VDH), to develop and implement an innovative mobile health intervention for people with HIV. PL has been adopted as usual care at the HIV clinic here at UVA and is expanding to other sites in Virginia, other states, and internationally. Within our Division, Dr. Flickinger is working with colleagues in geriatrics (Dr. Archbald-Pannone) on telehealth implementation for older adults, especially those in rural areas and congregate care settings. She is also collaborating with colleagues in the schools of Engineering and Nursing on developing natural language processing (NLP) methods for analyzing communication between patients and their care teams. She is seeking NIH funding for that project.
Prior to joining the UVA faculty, Dr. Memari completed the Academic Clinician-Educator Scholars fellowship at the University of Pittsburgh Medical Center, obtaining a Master of Science in Medical Education degree during the fellowship. Dr. Memari has previously published works on high-value care, social determinants of health, and growth mindset in medical education. His current research interests include studying the impact of educational methods and assessment of complex competencies, including communication skill development and self-regulated learning. His work has been published in Academic Medicine, the American Journal of Medicine, the Journal of General Internal Medicine, and the Journal of Hospital Medicine, among others.
Awards
Department of Medicine Awards
Bethany Payne NP, was selected by IM residents as NP of the year.
Zach Boggs MD, was selected by IM residents as Outpatient attending of the year.
Department of Medicine Excellence Awards
Maria Badaracco MD – Clinical Excellence
Jeannine Engel MD – Clinical Excellence
Stewart Babbott MD – Mentoring Excellence
Cindy Peery – Administrative Excellence
SOM Awards
Lien Dame MD – Deans Award Clinical Excellence
Christina Tieu MD – Deans Award Teaching
Rachel Kon MD – GME Master Educator Award
Andrew Parsons MD – Herbert S. Waxman Award for Outstanding Medical Student Educator
Promotions
David Callender MD – to Associate Professor
Brian Uthlaut MD – to Professor
Welcome To New Faculty
Alexandra Schwab MD, Dr. Schwab is a 2024 graduate of the UVA Internal Medicine Residency. She has joined the Division of General, Geriatric, and Palliative Medicine at 50% effort and the Division of Hospital Medicine at 50% effort for this academic year. Dr. Schwab will divide her ambulatory effort between University Physicians Orange and University Medical Associates. Dr. Schwab is co-directing the new Suboxone Clinic at University Medical Associates with Dr. Rachel Kon and one of the Chief Residents, Dr. Thompson Barr.
Laura Mitchell MD, Dr. Laura Mitchell is a 2022 UVA Internal Medicine Residency graduate and a 2022-2023 Chief Resident in the UVA Internal Medicine Residency who returns to UVA after one year of Endocrine Fellowship. Dr. Mitchell is teaching and practicing at University Medical Associates and is the Associate Medical Director of University Medical Associates. She will also round on the General Medicine Teaching Service.
Aislin Camoney MD, Dr. Aislin Camoney is a 2024 graduate of the UVA Internal Medicine Residency. She is full-time at University Physicians Charlottesville in direct patient care and teaching students and residents at UPC. She will also round on the General Medicine Teaching Service.
Margaret Hayden MD, Dr. Margaret Hayden is a 2022 Brigham and Women’s Hospital Internal Medicine Residency Program graduate. She earned her Master’s in Philosophy in Medical Anthropology from the University of Oxford as a Rhodes Scholar in 2015. Between 2022 and 2024, she worked as a physician in the Equal Justice Initiative in Montgomery, Alabama. She and her husband, Dr. Sanjay Kishore helped lead a team that established a free clinic that provided transitional primary care to individuals recently released from prison and jail. They helped develop and operate a mobile clinic. They visited parole centers across Alabama and developed point-of-care laboratory testing for Hepatitis C for a diagnosis and treatment program. They were Assistant Professors at the University of Alabama at Birmingham. She and Dr. Sanjay Kishore (Hospital Medicine) are joining in September. Dr. Hayden will divide her time between University Medical Associates (teaching and direct patient care) and as the Associate Director of the Center for Health, Humanities, and Ethics (Dr. Justin Mutter, Director).
Benjamin Cahill MD, Dr. Benjamin Cahill joined the Section of Geriatrics in July 2024. Dr. Cahill completed his residency training in Internal Medicine and his fellowship in geriatrics at the University of Virginia. Dr. Cahill joins UVA Geriatrics as part of the clinical team at Westminster Canterbury of the Blue Ridge and leads the geriatric outpatient consultation service at Charlottesville’s Veterans Affairs clinic. Dr. Cahill also serves as an assistant director of the PCOM clerkship.
Matthew Van Dongen MD, Dr. Matthew Van Dongen joined the Section of Geriatrics in August 2024. Dr. Van Dongen completed his residency training in Internal Medicine at the University of North Carolina – Chapel Hill and tripartite fellowship training in geriatrics, behavioral neurology and neuropsychiatry, and medical education – all at the University of Pennsylvania. Dr. Van Dongen is leading a new role for UVA Geriatrics in inpatient consultation on the trauma service and serving as core clinical faculty in the UVA Memory and Aging Care Clinic. He will also attend the General Medicine Teaching Service.
Elizabeth Cobb DNP, Dr. Elizabeth Cobb joined the Section of Geriatrics in January 2024. Dr. Cobb completed her Doctor of Nursing Practice at VCU School of Nursing and the FNP program at the University of Virginia. She has extensive experience working with older adults, having served as an APP with Hospice of the Piedmont and Valley Family and Elder Care in central Virginia. Dr. Cobb is working at Westminster Canterbury of the Blue Ridge, caring for patients throughout the continuum of care.
Hailey Vest, DO, Dr. Vest completed her Palliative Care fellowship at Cleveland Clinic in 2023 and has been a palliative care physician there. She will be joining the inpatient palliative consultation service in November or 2024.
Sarah Verga DO, did her palliative care fellowship at UVA in 2018 and worked as a palliative care physician at Sentara in Virginia Beach. She came back to UVA to work in the palliative care clinic in August 2024
Katie Waybill MD, Dr. Waybill completed her pulmonary critical care fellowship at Tufts in 2023 and did a palliative care fellowship at Beth Israel Deaconess Medical Center in 2024. At UVA, her primary appointment will be in pulmonary/critical care. Still, she will work one day a week in the palliative care clinic, focusing on pulmonary palliative care.
Meredith Davis NP, completed her NP degree at the University of Pennsylvania and has outpatient and inpatient palliative care experience at Fox-Chase Cancer Center and Cooper Union Hospital.
Achievements and Events
 Andrew Wolf MD
Andrew Wolf MD
Dr Andrew “Andy” Wolf has retired after 28 years of service at UVA. He was the Harry T Peters Sr Professor of Medicine. Dr. Wolf is much beloved and known for his infectious enthusiasm and expertise in medical education, having won the Internal Medicine Outpatient Attending of The Year 14 times (each year he was eligible to receive it). Dr Wolf is not only a consummate primary care internist, having been named a master in the ACP, but is also internationally known for his work in cancer screening. He has led the American Cancer Society Committee on cancer screening guidelines, which has led to genuine advances in cancer screening that have saved thousands of lives nationally. Andy will be missed for his hilarious humor, which he shared avidly with patients, trainees, and colleagues daily. Thankfully, Andy will be helping our Division in retirement and volunteering at the Charlottesville Free Clinic to precept residents and students rotating there.
 Stewart Babbott MD
Stewart Babbott MD
Dr Stewart “Stew” Babbott will be retiring in January 2025. Dr Babbott joined our faculty eight years ago from the University of Kansas to serve as Section Chief for General Internal Medicine. Stew is recognized as a national leader in primary care, serving on many national societies devoted to improving care of and training in Primary Care General Internal Medicine. While providing outstanding care to his patients, having been named a master in the ACP, Stew has also been a vocal advocate for faculty in our Division and department, leading efforts in faculty development. We will miss his affable nature and strong advocacy as he retires.
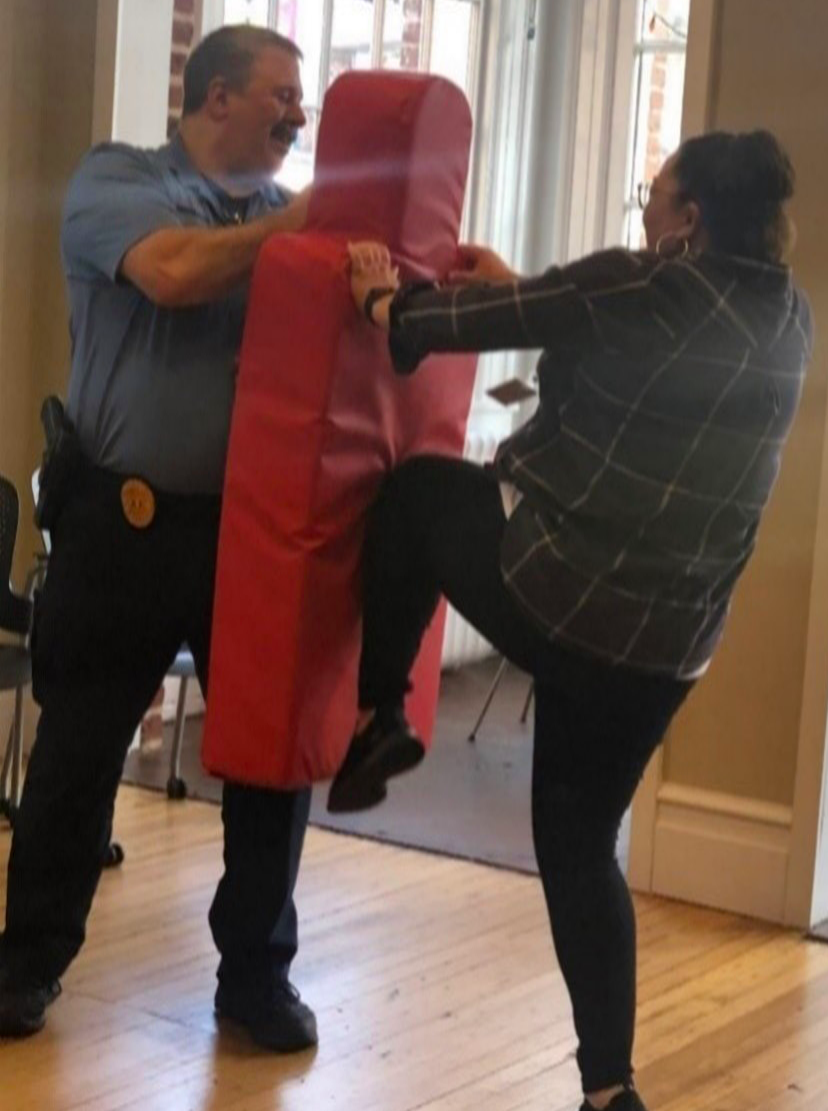
Beth Tyree in action during a Division-sponsored self-defense class.

Gray Herndon, Marcia Washington, Cindy Peery, Brigitte Binard, Sonja Spradlin at a staff luncheon.
GRANTS
Tabor Flickinger
Foundation: Betty Irene Moore Nurse Leaders and Innovators Grant (LeBaron)
VDH: Statewide Innovations (Ingersoll); Virginia IMPACT (Archbald-Pannone)
NIH: R01 MH122375 NIMH (Castel, Ingersoll)
NIH: R01 submission (Flickinger); R34 submission (Ingersoll)
Laurie Archbald-Pannone
The Gary and Mary West Health Institute Collaborative Grant, “Collaborative for Telehealth and Aging.”
Coulter Translational Partnership, “Model-driven design of microbial therapies to resolve C.
difficile infection.” PI: Jason Papin (BME), L Archbald-Pannone (DOM), Co-I Glynis Kolling (BME).
$153,000, 9/1/2023-8/31/2024, NCE until 2025 (Grant support: 3% FTE/year).
Virginia Long-Term Care Infrastructure Pilot Projects (VLIPP) – HAIAR, CDC Nursing Home Strike force
funding: Virginia Infection Control Center of Excellence (VICE), total estimated funding of $1,210,312 over two years ($ 605,156 with one, one-year renewal period, (Grant support: PI: 20% FTE/ year).
The Gary and Mary West Health Institute Collaborative Grant, “UVA-WHI Geriatric Telemedicine Resource Development” $265,000 award over two years (Grant support: PI 12-15% FTE/year).
The Gary and Mary West Health Institute Collaborative Grant, “Collaborative for Telehealth and Aging.”
Coulter Translational Partnership, “Model-driven design of microbial therapies to resolve C. difficile infection.” PI: Jason Papin (BME), L Archbald-Pannone (DOM), Co-I Glynis Kolling (BME). $153,000, 9/1/2023-8/31/2024, NCE until 2025 (Grant support: 3% FTE/year).
Prime, INC Course Director, “Enhancing Vaccine Uptake in Older Adults: Supporting Conversations With Your Patients.” And “Engaging Older Adults in Vaccine Education: A Toolkit for Healthcare Providers.”
Virginia Long-Term Care Infrastructure Pilot Projects (VLIPP) – HAIAR, CDC Nursing Home Strike force funding: Virginia Infection Control Center of Excellence (VICE), total estimated funding of $1,210,312 over two years ($ 605,156 with one, one-year renewal period, (Grant support: PI: 20% FTE/year).
Leslie Blackhall
NINR RO1: Characterizing the complexity of cancer pain in the home context by leveraging smart health technology. Role: Co-I. 2/1/21-11/30/25. $3,419,796
PCORI: REACH PC: Comparative Effectiveness of Early Integrated Telehealth Versus In-Person Palliative Care for Patients with Advanced Lung Cancer Role: Co-Investigator and Site Lead for multi-site national study 1/2018 – 1/2024
$10,957,491.
Betty Irene Moore Fellowship for Nurse Leaders and Innovators: Developing and Testing a Novel Mobile Health Solution (CommSense) to Improve Patient-Provider Communication Role: Co-I (Virginia LeBaron, PI) Amount: $450,000 Dates: 7/1/23 – 6/30/26
Go to Full October 2024 Issue of Medicine Matters
Filed Under: Basic Research, Clinical Research, Education, In the Know, News and Notes, Notable Achievements, Publications, Research, Top News