By Dr. Jonathan Swanson, Chief Quality Officer for Children’s Services, NICU Medical Director

Dr. Jonathan Swanson
If you have walked around any of the inpatient units over the last few weeks, you know that one of the major hurdles we currently face within the Children’s Hospital is space. At the turn of the year, we recently had the Pediatric Intensive Care Unit full with 17 patients, the Neonatal Intensive Care Unit over capacity with 54 babies, and the Acute care wards full with 39 patients. (If you are not aware, the PICU is currently staffed for 17 patients, the NICU for 51 patients and Acute Care for 39 patients). On top of this, the Pediatric Emergency Department was boarding another 3-4 patients waiting for a room on the 7th floor. Needless to say, with the rates of influenza and respiratory syncytial virus increasing over the last few weeks and likely continuing to increase over the winter, the availability for beds will be at an all-time high. This could potentially lead to cancelling procedures and planned admissions. Not what we desire for our patients.
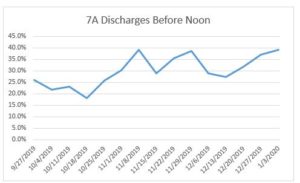
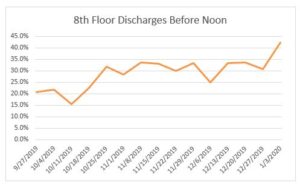
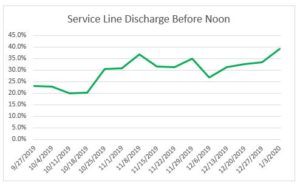
Over the last few months, the inpatient units have been working on the Wildly Important Goal (WIG) of increasing the number of patients discharged from the hospital by noon. The rationale is that getting patients out earlier in the day will allow improved patient flow and provide a better understanding of what beds are available earlier in the day, decreasing the likelihood, and need, for canceling planned admissions and procedures. Each unit looked at the problem (late discharges) from their own perspective to develop action items that may lead to the desired outcome. The SMART aim for the Children’s Hospital was “To increase the number of patients discharged by noon from 20% to 40% by December 31st.” So what did we do?
On 7Acute, the team followed the data and found that if the patient was successful in leaving by noon, they were much more likely to have a discharge order in by 10 AM. With that knowledge, Dr. Lynn McDaniel led the group by providing data to the various services on how they were doing with placing discharge orders by 10 AM. As this increased, so did the number of patients that were discharged by noon. Women’s Services (including newborn discharges) had similar findings and worked on improving throughput and coordination of care between OB and Pediatrics.
So how did we do? With 7Acute and the 8th floor accounting for 94% of Service Line discharges, those two units led the charge. In late September, approximately 20% of discharges were out before noon. At the end of the calendar year, 39% of the patients were discharged by noon. Although not quite reaching our goal of 40%, one can see the value of using data to find the problem and then attacking that problem to make an improvement.
If you have any more questions about this WIG or any other Service Line quality initiative, don’t hesitate to ask me or your unit/clinic Unit Based Leadership Team!
Filed Under: Features
