UVA is Magnet! (What does that mean for quality outcomes?):
On Monday, May 18th, the Health System learned that UVA re-achieved Magnet® status! The Magnet Recognition Program by the American Nurses Credentialing Center (ANCC) “recognizes healthcare organizations for quality patient care, nursing excellence and innovations in professional nursing practice.” According to the American Hospital Association, approximately 7% of hospitals in the United States have achieved Magnet recognition status. During the phone call announcing the recognition, the Be Safe program was cited as an exemplary process to improve patient outcomes. The ANCC notes that Magnet hospitals have “higher percentages of satisfied RNs, lower RN turnover and vacancy, improved clinical outcomes and improved patient satisfaction.”
So what evidence is there that Magnet recognition achieves “improved patient outcomes?” In this month’s journal Medical Care (Vol 53, pg 550-7), Dr. Kutney-Lee and co-authors looked at 136 hospitals in Pennsylvania between 1999 and 2006. They compared hospitals that achieved Magnet (11 hospitals) during the time period to those who did not (125 hospitals). In 1999, patient outcomes (specifically 30-day surgical mortality and failure to rescue) were not different between the two types of hospitals. By 2006, although all hospitals improved, Magnet hospitals outcomes were significantly better than their counterparts. Magnet hospitals had nearly 4 fewer deaths per 1000 patients. In the world of pediatrics, hospitals have used the Magnet model to implement changes in oral feeding practices in the neonatal intensive care unit leading to decreased length of stay, and several studies have demonstrated an improvement in patient satisfaction scores after Magnet recognition. Although it may be some time before we see clinical outcome changes, between the combination of Be Safe and Magnet recognition, UVA Children’s Hospital is well on its way to be the leading pediatric provider in Virginia
NICU Simulates Rare Procedures:
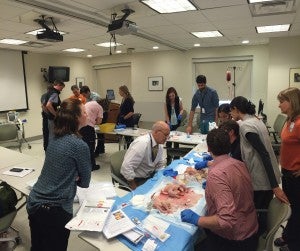
Simulation. We hear about it quite frequently when discussing medical student, resident and fellow education, however it is rare to see board-certified physicians simulating procedures in their specialty. During the most recent completion of the US News & World Report Best Children’s Hospital survey, one of the questions queried how many faculty had completed simulation within the last two years on procedures that were infrequently done. Although the answer this year was 0%, it provided the impetus for Dr. Brooke Vergales to develop a “skills day” exercise for faculty, fellows, nurse practitioners, NETS clinicians and even an aspiring PICU fellow. The participants practiced five relatively rare procedures (cardioversion, pericardiocentesis, exchange transfusion, pigtail catheter placement and chest tube placement) over the afternoon in early May. A fellow and faculty collaborator developed each of the stations. These teams then walked all of the participants through the station creating “standard work” for the procedure. Everyone that participated thoroughly enjoyed the time and thought it was a great refresher for those procedures that are less frequently performed.

Dr. Matthew Harer (2nd Year NICU fellow) demonstrating pericardiocentesis while Drs. Sinkin, Vergales and Zanelli look on.
Filed Under: Features
Tags: jrs3yc