Christopher Scott, MD
The University of Virginia’s commitment to advancing surgical education is exemplified by its latest initiative, the Robotic Surgery Bootcamp. This boot camp is part of a revamped curriculum designed to provide all residents and fellows with the skills necessary for proficiency in robotic surgery. Christopher Scott, MD, an associate professor in the Department of Surgery and the director of the program, sheds light on this new initiative and the technology that is transforming the future of surgical practice.
What was your role in organizing the Robotics Boot Camp?
UVA has had a comprehensive robotic surgery training program in place for several years; however, as robotic surgery has evolved and grown, there was a need to modify and improve upon the existing curriculum. I was appointed to lead a team of UVA robotic surgeons to “revamp” this curriculum. As director of the program, my role involved planning and putting together the curriculum and educational activities, as well as working with our partners at Intuitive Surgical to secure the necessary resources, i.e. robotics training platform, animal tissue models, cadaveric supplies, and simulation models. We took important feedback from our residents and fellows when implementing this most recent change in curriculum.
What skills are taught?
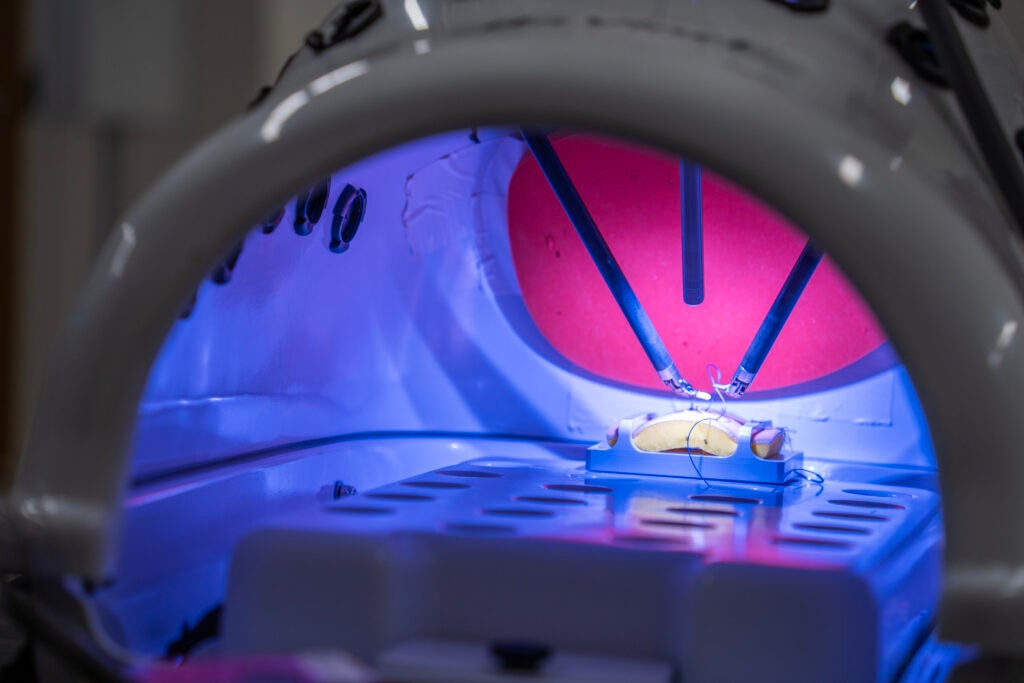
This is a comprehensive course built to the needs of each particular level of training. For the most junior level trainees, we cover the basics of robotic surgery, including the basic components of the robotic system, handling the robot, docking and undocking procedures, and beside assisting. For intermediate level trainees, we focus on simulation-based training and simulation models to practice skills such as economy in instrument motion and basic suturing and knot tying. For our more advanced trainees, we perform tissue and cadaveric-based training in which we simulate routine robotic operations, i.e. hernia repair, bowel anastomosis, and anatomic pulmonary resection.
Who receives this training?
All residents and fellows within the Department of Surgery receive this training, including general surgery residents, transplant fellows, traditional cardiothoracic fellows, I-6 integrated cardiothoracic residents, and urological surgery trainees.
What is the timeline for becoming proficient in robotic surgery?
The UVA Robotic Surgery Boot Camp runs for an entire week, Monday through Friday, so that we can accommodate the large number of residents and fellows in small groups to maximize the learning environment. At the time of their graduation from the General Surgery program, our trainees are proficient in performing robotic surgery independently and are granted a certificate that allows them to continue performing robotic surgery in their future practice.
What is it like to operate the DaVinci robot?
In some ways, it feels similar to participating in a very high-level augmented reality experience. The visualization is superb, with the ability for 3-dimensional high-definition optics. The hand controls are incredibly precise and engineered for quick adaptation. While there is no tactile feedback provided through the instrument controls on the DaVinci robot, your eyes quickly learn to perceive and interpret what your hands are typically doing during conventional open surgery.
What are the advantages and disadvantages of robotic surgery?
The advantages of robotic surgery are the ability to expand the capability of minimally invasive surgery to increasingly more complex cases – the superior visualization and precision of movement are important aspects of this. Furthermore, it is an excellent tool in our mission to educate and train the next generation of surgeon leaders. The disadvantages involve the limitations of minimally invasive surgery – there will always be situations in which minimally invasive surgery is not safe and/or feasible to perform and it will be important for surgeons to understand these implications and have the training/foundation to provide safe alternative approaches when necessary.
What surgical specialties have been most impacted by robotics?
Robotic surgery is currently impacting every field of surgery. Recently, it has seen particularly explosive growth in the field of general surgery, transplant surgery, surgical oncology, and thoracic surgery. For example, in my field of Thoracic Surgery, the robotic approach has now become the most common approach to performing a lobectomy, which is removal of one of the lobes of the lung, usually due to cancer. This is unique in that since the inception of lung surgery in the US nearly 100 years ago, the open approach has always been the most common approach to lung cancer surgery. This has changed just within the past few years as a result of robotic technology.
How do you expect the field of surgical robotics to evolve?
We are currently on the 4th generation of the DaVinci robot. Like all technology, there is continued ongoing refinement in instrumentation, ultimately enabling less invasive approaches. We are currently understanding the use of a single port robotic system in which the surgery is performed through a single incision. Furthermore, with the advancement of artificial intelligence and machine learning, the field is poised to explore how these technologies can improve patient safety, reduce errors/complications, and increase the ability to teach and train.
How has robotic surgery impacted surgical care at UVA?
For my particular program, Thoracic Surgery, we have quintupled the volume of robotic cases since I was recruited here to UVA in 2021. Although it’s not completely linear, the amount of open/conventional surgery has decreased. Less open surgery typically means less time in hospital, fewer complications, less pain, and a quicker return to life for patients. From my practice perspective, there are many stories of patients having complex robotic surgery and quickly getting back to work, to their families, and to their passions.
Christopher Scott, MD is an associate professor in the at the School of Medicine’s Department of Surgery, who specializes in robotic-assisted, minimally invasive thoracic surgery, as well as end-stage lung disease, lung transplantation, and pulmonary thromboendarterectomy for CTEPH.
Article by Holly Atkinson. Contributed photos.
Filed Under: Education