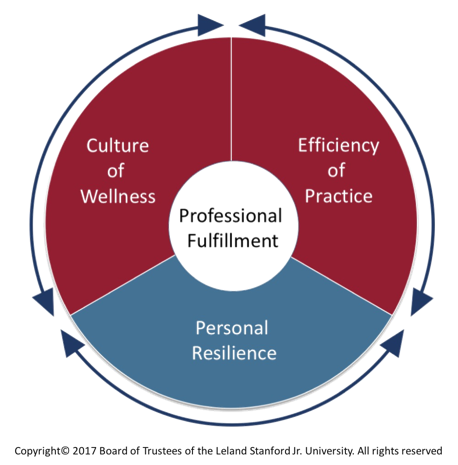
Clinician Wellbeing, Efficiency of Practice, Ambulatory Optimization and the Be Wise Approach
Stewart Babbott, MD a UVA Professor in the Department of Medicine researches and writes on clinician well-being. He is one of the authors in a recent article on physician wellbeing…
Epic Training is Happening Now
Dear Colleagues, Epic Training is Happening Now When you think of Epic Phase 2, are you wondering: Will I be impacted? What’s changing as a result of Epic Phase 2?…
Positive Comments May 1 to December 1, 2016
Positive Comments from our patient satisfaction surveys can be viewed by clicking the link. To find a provider name or keyword, use CTRL+F to bring up the search utility.
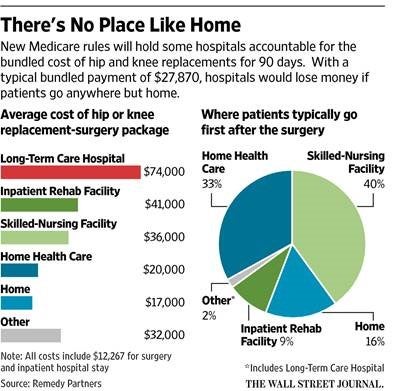
The Impact of Bundled Payments
After seeing this headline in the news: “CMS Announces Bundled Payments for Joint Replacement Surgery”, my neighbor told me that he was going to need to hurry to have his…
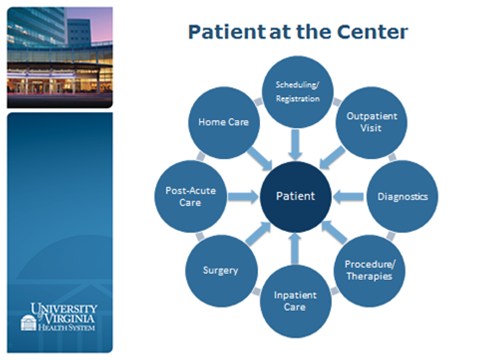
Service Lines: Putting Patients at the Center of Their Care
Nationally, we are observing that many major medical centers are using service lines to manage their clinical operations. The American Association of Medical College’s Advisory Panel on Health Care has…
Becoming Our Patient’s “Pharmacy Home”
We've had a lot of interest in our most recent blog post and wanted to share some additional thoughts from the Director of Pharmacy, Rafael Saenz. One writer acknowledged that…