Message from Division Chief Mohan Nadkarni, MD, Division of General, Geriatric and Palliative Medicine
 I am pleased to highlight exciting programs and faculty for our busy Division. We have a broad array of faculty, APPs, and staff whose clinical care, education, and scholarship span the breadth of Internal Medicine. We see a diverse range of patients on a longitudinal basis across various settings. Educationally, we are the backbone of GME and UME medical training, providing three-year mentorship to our IM residents at University Medical Associates and University Physicians Charlottesville, as well as vital training in Geriatrics and Palliative care. Many faculty also provide four-year mentoring to medical students via the FCM course. Our Palliative and Geriatric sections also host vibrant fellowship programs. We have enhanced scholarship activities with new research directors (Tabor Flickinger and Milad Memari) for the Division, as well as strategic planning retreats to improve faculty development offerings. We highlight the new Suboxone clinic at UMA, the opening of the new geriatrics clinic at Riverside, the new geriatrics trauma consult service, the addition of a palliative/pulmonary collaboration, and welcome Dr. John Moriarty as our new Section Head of GIM and Dr. Dacre Knight, who will lead the new Ehlers-Danlos center. I am profoundly thankful and impressed by the tremendous and varied care, education, and research our Division provides. I appreciate the collaborations with our sister divisions within our supportive Department of Medicine.
I am pleased to highlight exciting programs and faculty for our busy Division. We have a broad array of faculty, APPs, and staff whose clinical care, education, and scholarship span the breadth of Internal Medicine. We see a diverse range of patients on a longitudinal basis across various settings. Educationally, we are the backbone of GME and UME medical training, providing three-year mentorship to our IM residents at University Medical Associates and University Physicians Charlottesville, as well as vital training in Geriatrics and Palliative care. Many faculty also provide four-year mentoring to medical students via the FCM course. Our Palliative and Geriatric sections also host vibrant fellowship programs. We have enhanced scholarship activities with new research directors (Tabor Flickinger and Milad Memari) for the Division, as well as strategic planning retreats to improve faculty development offerings. We highlight the new Suboxone clinic at UMA, the opening of the new geriatrics clinic at Riverside, the new geriatrics trauma consult service, the addition of a palliative/pulmonary collaboration, and welcome Dr. John Moriarty as our new Section Head of GIM and Dr. Dacre Knight, who will lead the new Ehlers-Danlos center. I am profoundly thankful and impressed by the tremendous and varied care, education, and research our Division provides. I appreciate the collaborations with our sister divisions within our supportive Department of Medicine.
Mohan Nadkarni, MD
CLINICAL UPDATE
 GENERAL MEDICINE
GENERAL MEDICINE
by Rachel Kon, MD
Rotating to a safer opioid: Patients receive concurrent Chronic Pain and Opioid Use Disorder treatment as IM Residents gain experience prescribing Buprenorphine in the UMA Office-Based Opioid Treatment (OBOT) Program
The University Medical Associates Office-Based Opioid Treatment (OBOT) program is now in its second year of operation, meeting weekly in the resident primary care continuity clinic at the University of Virginia. We are seeing both established and new patients for management of Opioid Use Disorder (OUD) or co-occurring chronic pain and OUD with Buprenorphine. If an opioid is needed, Buprenorphine is now the preferred first-line opioid for chronic pain when multi-modal non-opioid treatments for the pain source have been exhausted by the 2022 Veterans Administration Opioid Treatment guidelines. This is due to Buprenorphine’s equal analgesic potency to other opioids, low abuse potential, and its favorable safety profile: reduced respiratory depression, lower fall risk and cognitive effects in the elderly, and reduced constipation, immunosuppression, sexual dysfunction, and sarcopenia compared with full-agonist opioids.
In our first year, we received a variety of referrals for OUD treatment that also involved another substance use disorder. We are now supporting our primary care patients in this dedicated weekly session for alcohol use disorder and cocaine use disorder treatment in addition to OUD. UMA OBOT has a dedicated RN coordinator, pharmacist, and social work partners available to provide patients seeking care for substance use disorders with frequent and multi-disciplinary support. Our IM residents participate at the center of the care team to see how patients can recover from their substance use disorder with proper treatment and support.

Margaret Hayden, MD
Implementing this new program and refining our workflows was led by Dr. Allie Schwab during her year with the

Matt Allen, MD
General Internal Medicine department, before she headed to a fellowship in rheumatology at Duke University. With her departure, Dr. Rachel Kon will direct the program with the intention of understanding how this experience for the residents fits into their larger OUD Treatment thread within the IM residency ambulatory curriculum. This academic year, we have welcomed three new clinical preceptors to the program: Dr. Margaret Hayden, Dr. Matt Allen, and Dr. John Moriarty. Dr. Hayden treated patients with Buprenorphine for OUD during her residency at Brigham and Women’s Hospital and then started a free mobile Hepatitis C and OUD treatment program in Montgomery, Alabama, during her first faculty position at UAB. Dr. Moriarty precepted in a similar embedded OUD treatment program in the Yale Primary Care Track continuity clinic before he arrived at UVA. Dr. Allen runs our outreach clinic for unhoused patients at the Haven and treats complex patients with chronic pain in the UVA HOME program. Together, the breadth and depth of their experience are enriching the educational experience for our residents.

John Moriarty, MD
In our first year, we saw patients experience treatment success – getting back to full-time work, being able to spend time with family without having withdrawal symptoms, and having their chronic pain controlled to a point where they can function in their lives. Several patients have graduated back to their PCPs for ongoing management. Patients with OUD who are ready to start treatment but do not have a PCP can be referred to UMA OBOT for both an outpatient buprenorphine prescriber and a new PCP. Our PGY2 IM residents rotate through this session several times during the academic year to experience both initiating and titrating Suboxone for OUD and accruing 1-2 patients in OUD treatment for their continuity panel, thereby gaining experience in maintenance therapy.
Please send questions or patient referrals in EPIC via staff message to “P UMA OBOT REFERRALS” or email Rachel Kon directly. Melissa Warren is our RN Coordinator. We look forward to expanding this program to meet the patient and educational needs of UVA IM.
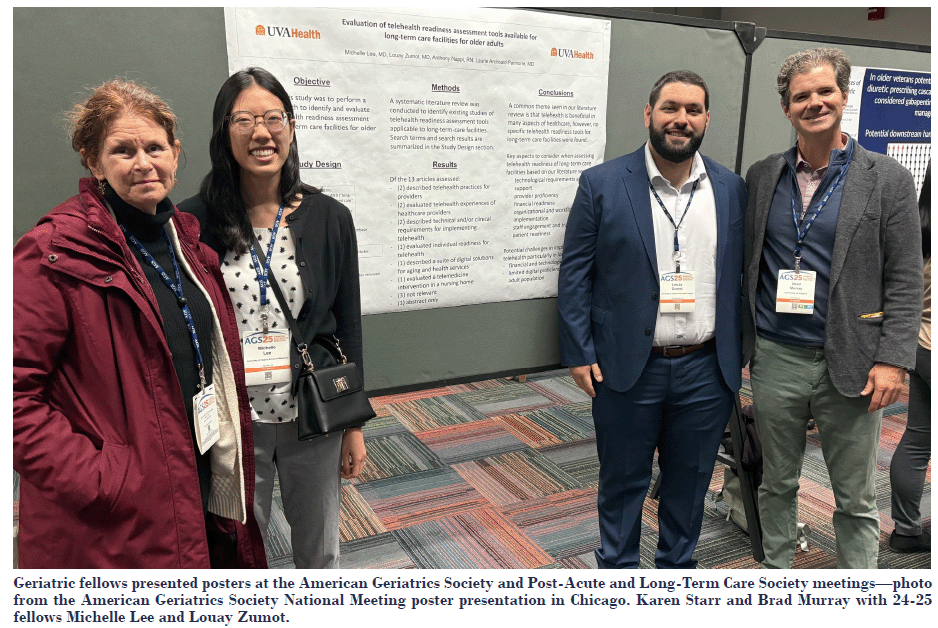
GERIATRICS

Laurie Archbald-Pannone, MD

Justin Mutter, MD
New JABA clinic opening at Riverside – To help the growing number of older adults access the specialized care they need, UVA Health plans to open an expanded geriatrics clinic in Albemarle County in December. The new clinic will be at 2325 Seminole Lane, Suite 300, in Albemarle County. The facility will have 12 examination rooms, two consultation rooms, and a treatment room. With the added space, Dr. Laurie Archbald-Pannone says they’ll be able to serve more patients.
“The Pew Research Center estimates that the number of Americans ages 100 and older will quadruple by 2054, so our team is excited to move into this new clinic space to ensure older adults in Central Virginia have convenient access to care tailored to their unique needs,” said Justin Mutter, MD, MSc, UVA Health’s section head for geriatric medicine.
“Access to health care is a critical piece of both managing our health conditions and maintaining healthy aging,” said Dr. Archbald-Pannone, geriatric physician at UVA Health.
Matthew J Van Dongen, MD
UVA Health Increasing Access to Geriatrics Care
The UVA Department of Surgery underwent an American College of Surgeons Trauma review this summer and was able to showcase a new partnership with the Geriatric Section. Dr. Matt Van Dongen collaborated with Dr. Matt Noorbakhsh to develop a Geriatric Consult Service, aiming to enhance care for seniors within the Trauma Service. Van Dongen, along with NP Jenn Conklin, has been assisting in safe discharges, establishing care goals, reducing polypharmacy, and lowering the risk of falls. They hope to expand the consultations to other surgery services in the future.
PALLIATIVE

Katie Waybill, MD
This year, Palliative Medicine welcomed Dr. Katie Waybill to UVA. She is board-certified in Palliative Care and Pulmonary-Critical Care. She works with our team one day a week in the clinic and has started a pulmonary palliative care program, which has been highly successful. In the past year, we have had 57 consultations referred to the pulmonary palliative clinic from all subspecialty clinics within pulmonary medicine. Our highest percentage of patients has either COPD or ILD. Dr. Waybill has developed a pathway for patients with COPD who have recurrent admissions or exacerbations, in collaboration with Dr. Michael Shim, on the advanced COPD team. Since the program began, 20 patients have been referred to hospice. Almost half are seen via telehealth due to difficulty accessing care, primarily related to distance and the challenges of traveling with oxygen.
RESEARCH UPDATE
Joshua Barkley, MD
The Division of General, Geriatric, and Palliative Medicine will continue to hold monthly Faculty Development meetings for Medical Education and Clinical Research in the 2025-26 Academic Year.
We plan to host Dr. Adam Sawatsky (Associate Professor of Medicine, Mayo Clinic) to speak to our Division and at DOM Grand Rounds on 2/20 in conjunction with the Department of Medicine.
The Section of Palliative Medicine continues to collaborate with Dr. Virginia LeBaron of the School of Nursing on several grants. Recruitment for the BESCI-C trial, which investigates the use of smart health technology in the home to assess and monitor cancer-related pain treatment, is now complete, and data analysis is ongoing. Dr. Joshua Barclay is leading a research project that surveyed palliative care programs nationwide about their involvement (or lack thereof) in caring for patients with sickle cell disease.
EDUCATIONAL UPDATE

Nat Timmins, MD

Haley Vest, DO
Palliative Medicine Fellowship, led by Dr. Nat Timmins, continues to thrive. Our team remains deeply committed to training skilled Hospice and Palliative Care clinicians as well as teaching primary palliative care skills. Faculty are involved in multiple educational initiatives through the UVA School of Medicine and regularly host medical students as well as trainees from Internal Medicine, Geriatrics, Hematology-Oncology, and Critical Care.
We’re also excited to announce the launch of a new longitudinal communication skills curriculum, developed by Dr. Haley Vest (Palliative Care) and Dr. Katie Waybill (Palliative Care/Pulmonary-Critical Care). Running from July 2025 to June 2026, the program brings together seven fellows from Palliative Care, Pulmonary/Critical Care, and Geriatrics for structured, skill-based training in challenging clinical communication. The curriculum includes opportunities for observed practice with direct feedback. We hope to expand participation for future years.
CHECK OUT THE DIVISION’S SECTIONS ON OUR WEBSITE
HIGHLIGHTS
AWARDS
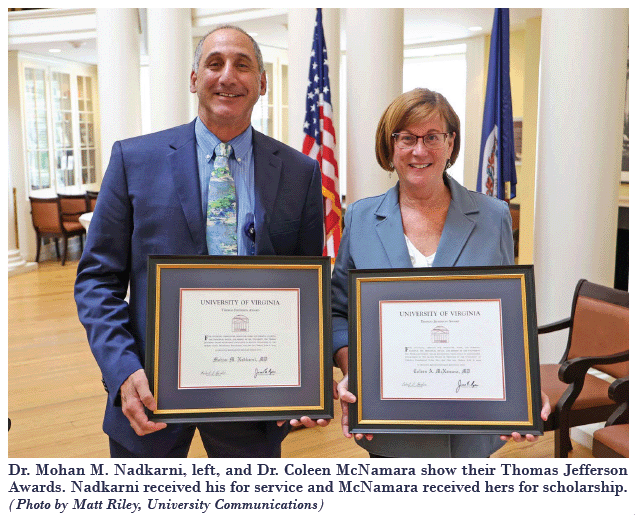
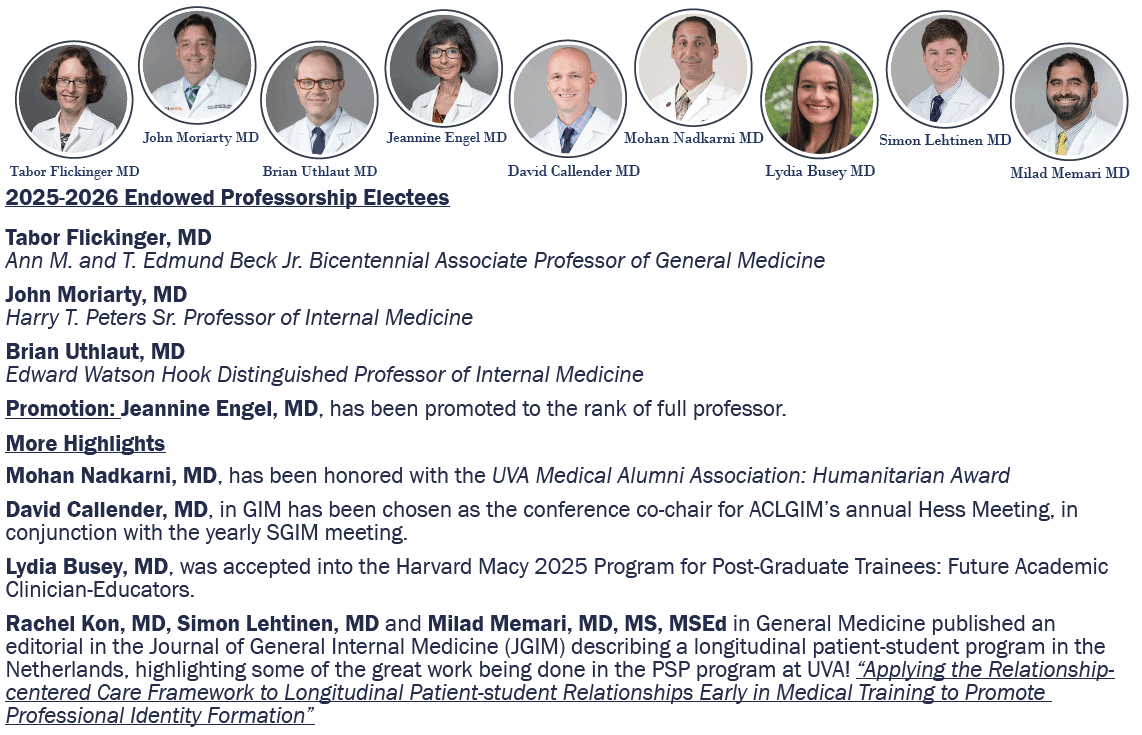
Mohan Nadkarni, MD – The Thomas Jefferson Award for Service was given to Dr. Nadkarni in recognition of over three decades of service to the University as a physician, educator, advocate, and community leader.
The Thomas Jefferson Awards have been presented annually to members of the University community since 1955.
In presenting the service award, then UVA President Jim Ryan noted Nadkarni’s efforts to provide medical services to all who need them, including co-founding the Charlottesville Free Clinic during his residency in 1992. He still volunteers at the clinic, which has become a cornerstone of care for the area’s uninsured.
Nadkarni also teaches Social Issues in Medicine, a course which has become a national model for integrating service learning and social determinants of health into medical school curriculum. He has served as a board member for the Blue Ridge Area Coalition for the Homeless, volunteered as a supervising physician at UVA’s Haven Homeless Clinic on the Downtown Mall, and helped plan and develop a new mobile community outreach project. Read more in UVAToday…

Darce Knight, MD
Dacre Knight, MD, has joined the Univeristy of Virginia Health as an associate professor of medicine and the medical director of the new UVA Health Ehlers-Danlos Syndrome (EDS) and Hypermobility Disorders Center. Dr. Knight previously served as medical director of the EDS Clinic at Mayo Clinic, which he founded in 2019 and successfully led to designation as a Center of Excellence in EDS care in 2023. Before his time at Mayo Clinic, he served as a physician in the U.S. Air Force. Dr. Knight is an active researcher and educator, currently supported by NIH R21 funding, and is a member of the International Consortium on EDS & HSD, affiliated with the Ehlers-Danlos Society.
He received the 2025 “The Pioneer in Clinical Care Award” from the EDS Society. This award honors a remarkable individual who has demonstrated a long-term commitment to outstanding care, research, and progression into Ehlers-Danlos syndromes, hypermobility spectrum disorders, and the associated symptoms and conditions. Lara Bloom, CNE, President and CEO”
EDS Center
The UVA Health EDS and Hypermobility Disorders Center is slated to open in early 2026 and will offer comprehensive, multidisciplinary care for patients with EDS and related conditions. Under the leadership of Dr. Knight, the center will coordinate complex care for patients within driving distance of Charlottesville and develop individualized care plans in collaboration with community providers for those traveling from farther away. Pediatric EDS care will continue under the leadership of Ina Stephens, MD, ensuring a seamless transition of care across all ages. The center is designed to integrate clinical care with cutting-edge translational research, advancing understanding and improving outcomes for individuals living with EDS.
Email address for the center: RUVAEDSCenter@uvahealth.org
We are actively accepting referrals to be placed on our waiting list via this email address.
 EVENTS
EVENTS
Strategic Retreats – January and June 2025
On January 31, 2025, the Division convened a strategic planning retreat to define our future direction and strengthen alignment with UVA Health’s broader mission. Through structured interviews and facilitated discussions, faculty and staff identified four core areas for strategic development: Supporting Faculty Thriving Together, Patient Care Experience, Career and Skill Development, and Administrative Support/Faculty Communication.
Over the subsequent months, working groups developed actionable initiatives, including a Division-wide intranet, structured faculty–administrator engagement, an advocacy forum, a holistic care board for complex cases, and enhanced pathways for faculty development and mentorship. A follow-up session on June 27 provided an opportunity to review progress, address any barriers, and confirm the next steps.
These outcomes reflect the Division’s commitment to operational excellence, faculty vitality, and the delivery of high-quality, patient-centered care. The process also reinforced our culture of collaboration and innovation, ensuring that our Division remains a leader within the Department of Medicine and UVA Health.
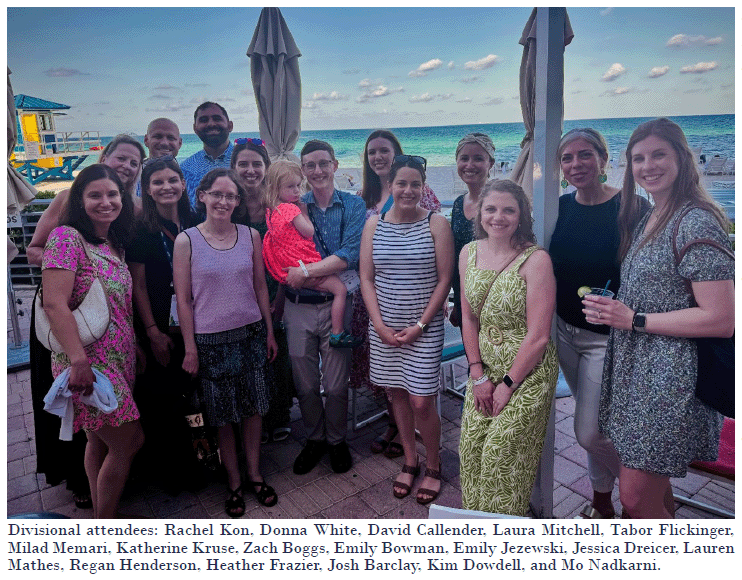 Society of General Internal Medicine’s Annual Meeting – Hollywood, Florida
Society of General Internal Medicine’s Annual Meeting – Hollywood, Florida
The Division of General, Geriatric, and Palliative Medicine was well represented at this year’s Society of General Internal Medicine Meeting. We had twenty attendees from UVA at the conference, who presented nine posters and nine other presentations, including workshops and panels, and played leadership roles in four interest groups. The presentations from UVA included contributions from at least eleven faculty members, six residents, three medical students, two nurses, and two pharmacists as co-authors. All this shows growth from prior years! This conference provided a valuable opportunity for our Division’s faculty, trainees, and interdisciplinary collaborators to share their scholarly work with a national audience, as well as engage in networking and mentorship.
Welcome hike in the Blue Ridge Mountains for John Moriarty with GIM faculty and family

Left to right: Susan Heald (Evan Heald’s wife), Laura Mitchell, David Callender, Carla Callender (David Callender’s wife), Evan Heald, John Moriarty, Margaret Hayden (holding her son) Dogs from left to right front row: Huntley, Mack, Mazie, and Charlie. Evan is holding Molly.
 WEDDING – David Callender, MD
WEDDING – David Callender, MD
David and Carla married on Saturday, June 21, 2025, with the ceremony in White Hall, Virginia, at Mount Fair Vineyard. It was attended by many of our general internal medicine colleagues and UMA staff. Pictured below are David, Carla, and their children, Miles (12) and Anna (15). Carla is from Charlottesville and is a nurse anesthetist here at UVA.
View the full issue of the October 2025
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, Expressions, In the Know, New Faces, New Places, News and Notes, Notable Achievements, Publications, Research, Top News