 I am so proud of our faculty and staff’s resilience and commitment to our mission. As the mighty challenges mount, they grow stronger and closer together as a team. Whether it is a funding line of eight in NIAID, delays in reviews and awards, constant turnover in clinic personnel, or uncertainties challenging our ASPIRE values and wellbeing, they adapt and overcome. They continue thriving, discovering, teaching, mentoring, and advancing the specialty.
I am so proud of our faculty and staff’s resilience and commitment to our mission. As the mighty challenges mount, they grow stronger and closer together as a team. Whether it is a funding line of eight in NIAID, delays in reviews and awards, constant turnover in clinic personnel, or uncertainties challenging our ASPIRE values and wellbeing, they adapt and overcome. They continue thriving, discovering, teaching, mentoring, and advancing the specialty.
Our faculty continues to conduct impactful research and publish it in high-profile journals. Glenda Canderan, PhD and, Lyndsey Muehling, PhD in the Woodfolk lab, and many collaborators across the institution just published their high-profile work on cellular mechanisms of injury in long COVID in Nature Immunology, garnering huge national attention. Jeffrey M. Wilson, MD, PhD, and Dr. Corrinne Keet from UNC were also featured nationally for their paper highlighting potential cardiovascular risks associated with food allergen sensitization. Emily C. McGowan, MD, PhD, along with her peds and adult GI colleagues, organized a highly successful inaugural statewide Eosinophilic Esophagitis (EoE) conference last Fall, hosted here at UVA’s Daren Hall.
Other faculty achievements also keep coming: Thomas Platts-Mills, FRS, received the Thomas Jefferson Scholarship Award last summer, one of the highest honors for researchers across the University of Virginia. Charlene Dunaway Altamirano, MD, PhD, joined our faculty after completing her fellowship in December and will continue her international food allergen sensitization work in the Platts-Mills lab. We are expecting good news on the promotions of Dr. McGowan and Dr. Wilson this year. In January, Judith Woodfolk, MBChB, started her term as co-Director of the MSTP program. Monica Lawrence, MD, is completing an immensely successful first year as institutional DIO, excelling under the most trying of circumstances. And, saving potentially the most exciting for last: Dr. Scott Smith has been recruited from Vanderbilt, arriving at UVA in August. Scott already has multiple collaborators at UVA and brings his unique monoclonal IgE platform for studying allergic and infectious diseases as a future addition to the Manning Institute.
Our training mission remains front and center for the Division. Sam Minnicozzi, MD, completed a banner first year as Program Director. We welcomed Nathan Richards, MD, and Amelia Perozo as new fellows this past year. We had another successful match with Natalie Eidson, DO, from MUSC, and Matt Scott, MD, from VCU, arriving this summer. Congratulations to our graduate students in the Woodfolk lab. Naomi Bryant successfully defended her thesis last month. Paul Dell received a 5th percentile score on his F31 and serves as BIMS student body vice president.
Finally, the 63rd Annual Oscar Swineford conference was a tremendous success, pairing our stellar faculty from multiple Departments and second-year fellows with nationally renowned speakers. Invited speakers included Anju Peters from Northwestern, Melanie Dispenza from Johns Hopkins, Len Bacharier from Vanderbilt, Ben Wright from the Mayo Clinic, Josh Kennedy from Arkansas Children’s, Tim Platts-Mills from Ophirex, Inc., and Dana Alban, MD, from the UVA PCCM Division.
I could go on, but find myself out of space. Just know that I am very proud of this division, which continues to excel as a team no matter the challenge.
~ Michael Nelson, MD PhD
CLINICAL
2024 Asthma, Allergy, and Immunology, Department of Medicine Awards

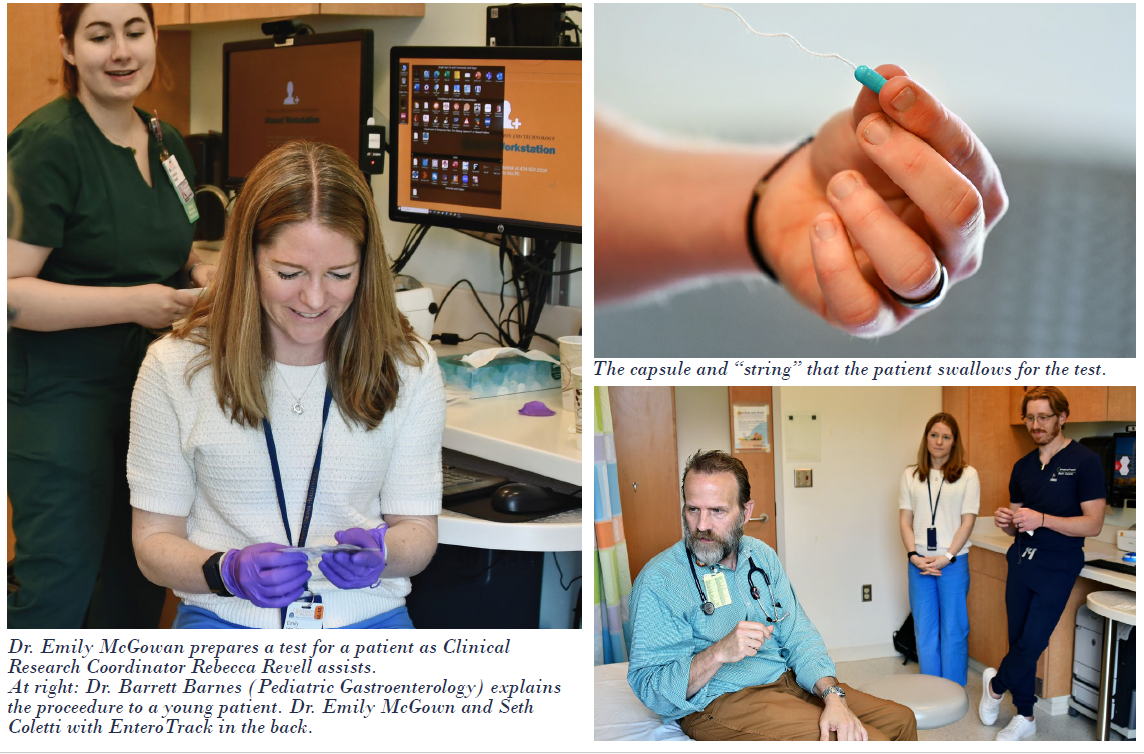
First Esophageal String Test In The State
On April 30, 2025, the University of Virginia became the first center in the State of Virginia to offer the esophageal string test, a novel, minimally invasive tool to assess for eosinophilic inflammation in the esophagus. Incorporating this test into clinical practice could minimize the need for patients to undergo recurrent endoscopy to monitor their eosinophilic esophagitis.
RESEARCH
From left, first row: MarthaJoy Spano, W. Gerald Teague, Larry Borish, Rebecca Revell, Khyati Menghani Back row: Kristin Wavell, Cameron Griffiths, and Elaine Etter
Borish Lab
The Borish [Larry Borish, MD] laboratory’s primary focus remains the role of rhinovirus (RV) in precipitating asthma exacerbations. These NIH-funded studies are designed to define the role of innate immune responses, including anti-viral and T2-promoting immune responses, by infected airway epithelial cells as they might distinguish the consequences of RV infections in asthmatics, allergic rhinitis, and healthy control subjects. The Borish laboratory is also the co-lead sponsor of a Regeneron-funded, investigator-initiated study entitled “Viral infection in asthma (VIA) Study.” This randomized, placebo-controlled study assesses cellular and molecular markers related to experimental RV infection in asthmatics and the effect of dupilumab in preventing exacerbations in this investigational model. This study will aim to assess the molecular and cellular basis by which dupilumab prevents the development of an RV-induced asthma exacerbation. Unrelated to the RV studies, the Borish lab collaborates closely with Dr. Gerry Teague in pediatrics as co-PI for studies addressing the role of mast cells and mononuclear phagocytic cells in the immune response to viral respiratory infections in children and adolescents with problematic wheeze.
Additional NIH-funded studies have identified an immune deficit state in the airways of many infants with a persistent wheeze that leads to susceptibility to persistent RV injection, chronic neutrophilic bronchoalveolitis, and increased susceptibility to the development of asthma. Finally, we are enrolling patients in a Regeneron-sponsored study to demonstrate the ability of dupilumab to attenuate staphylococcus aureus infection in chronic sinusitis and ameliorate the dysbiotic state, including with restoration of a healthier antimicrobial state, including restoration of a healthier antimicrobial state.

From left: Rebecca Revell, Emily McGowan, and Roopesh Singh
McGowan Lab
Dr. Emily McGowan’s group continues to expand their research on eosinophilic esophagitis (EoE), an emerging form of food allergy. Dr. McGowan established the University of Virginia EoE Cohort with her collaborators, Drs. Bryan Sauer (Adult Gastroenterology) and Barrett Barnes (Pediatric Gastroenterology). This cohort longitudinally follows over 350 patients with EoE and has been used to examine the immunologic drivers of this disease. In particular, her team found that immunoglobulin G4 (IgG4) may play an essential role in the inflammatory response in EoE. Through an NIH/NIAID R01 Award, they are examining whether this could be used to help identify food triggers in EoE patients. This work is being performed in collaboration with the laboratories of Dr. Judith Woodfolk (Allergy/Immunology) and Sarah Ewald (Microbiology).
Dr. McGowan’s group is also examining the epidemiology of EoE, as they have data suggesting that this condition may be underdiagnosed among patients with other allergic conditions and those with decreased access to care. This work is being performed in collaboration with Dr. Melissa Little (epidemiology) and Rebecca Revell (research coordinator).
Finally, Dr. Roopesh Singh (Assistant Professor, Research Scientist in the McGowan lab) has been investigating whether consuming processed milk could be a risk factor for the development and propagation of EoE. This work has been funded by the American College of Gastroenterology (PIs McGowan and Sauer), iTHRIV, and the NIH/NIAID (K23, R21, R01).
From left, Rishi Shah, Matthew MacCallum, Jeff Wilson, Thomas Platts-Mills, Pamela Schoppee Bortz, and Lisa Workman
Wilson and Platts-Mills Labs
Dr. Jeffrey Wilson and Dr. Thomas Platts-Mills have a major clinical and research focus on the alpha-gal syndrome. Their labs have been involved in NIH and DoD-funded studies to better understand tick-acquired allergic disorder’s epidemiology and risk factors. Based on a prior observation that alpha-gal IgE sensitization was associated with heart disease, the lab has also carried out NIH-funded studies assessing links between IgE antibodies to food and heart disease.
As part of these investigations, Dr. Wilson has ongoing collaborations with researchers inside and outside UVA, including Dr. Coleen McNamara (Cardiology/Beirne Carter Immunology Center) and Dr. Loren Erickson (Microbiology/Beirne Carter Immunology Center).

From left: Judith Woodfolk, Glenda Canderan, Lyndsey Muehling, Paul Dell, and Naomi Bryant
Woodfolk Lab
Dr. Judith Woodfolk’s lab continues to study immunity to respiratory viruses and allergens in diverse diseases using systems immunology methods. Her lab recently reported in Nature Immunology on distinct immune networks underlying the severity of lung injury after severe COVID-19 illness. This paper describes work done by an extensive interdisciplinary team of investigators inside and outside UVA, including joint first authors Drs. Glenda Canderan and Lyndsey Muehling (Division of Asthma, Allergy and Immunology), as well as investigators from the Division of Pulmonary and Critical Care Medicine (Drs. Catherine Bonham, Alexandra Kadl, and Jeffrey Sturek) and the Beirne B. Carter Center for Immunology Research (labs of Drs. Coleen McNamara and Jie Sun). The COVID project originated from an initiative spearheaded by the team early in the pandemic that garnered the 2021 Dean’s Award for Excellence in Team Science. The findings are significant for offering potential biomarkers of severity and new targets for treating lung disease in patients experiencing post-COVID sequelae. Dr. Woodfolk presented this work in a keynote lecture at the 2024 UVA Immunology Research Day.
The COVID project has led to work funded by an NIH/NIAID administrative supplement on biomarkers of Alzheimer’s disease in patients with systemic inflammatory programs (collaboration with Dr. Thomas Platts-Mills). It has also fostered a robust collaborative network involving work on ACE-2-like enzymatic activity in patients with persistent pulmonary symptoms (Dr. Steve Zeichner, Department of Pediatrics), sexual dimorphism of chimeric RNAs (Dr. Hui Li, Department of Pathology), and mathematical modeling of infection outcomes (Dr. Rayanne Luke, George Mason University; and Dr. Prajakta Bedekar, Johns Hopkins University/NIST). Beyond working on the immunology of COVID illness, the lab continues its research with Dr. Larry Borish on the effects of IL-4Ralpha blockade on the response to rhinovirus challenge and with Dr. Emily McGowan on T-cell mechanisms of eosinophilic esophagitis.
In lab news, Naomi Bryant, a BIMS graduate student working with Dr. Gerry Teague (Department of Pediatrics), has completed her thesis work on rhinovirus as a driver of T-cell dynamics in the lower airways of children with severe asthma. Her work has been accepted for publication in JCI Insight, and she successfully defended her thesis in April. Paul Dell, another BIMS graduate student, presented his work on atypical B cells in severe asthma in a Featured Poster session at the 2025 AAAAI annual meeting. In career advancement initiatives, Dr. Muehling participated in the AAAAI Faculty Development Program held in Milwaukee, WI, in September 2024.
In January 2025, Dr. Woodfolk was appointed Co-Director of the UVA Medical Scientist Training Program. She will lead the Program with Dr. Mariano Garcia-Blanco (Chair, Department of Microbiology, Immunology and Cancer Biology). Dr. Woodfolk continues to serve as a chartered NIH IHD Study Section member.
The Woodfolk lab continues to seek new scientific partnerships inside and outside UVA and extends thanks to all involved in their collaborative ventures!
The 63rd Annual Swineford Allergy Conference
EDUCATION
Our long-standing fellowship program continues to celebrate the many achievements of our fellows-in-training. We congratulate our 2025 graduating fellows, Dr. Thomas Offerle, who will be joining Asthma and Allergy Specialists North Carolina, and Dr. Samantha Nguyen, who will be joining Whole Family Allergy and Immunotherapy, Maryland. In July 2024, we welcomed two new fellows into the program: Dr. Maria Amelia Perozo (Danbury Hospital, Internal Medicine) and Dr. Nathan Richards (Harnett Health, Internal Medicine). We also completed another very successful virtual recruitment season and are excited to welcome two new incoming fellows in July 2025: Dr. Natalie Eidson (Medical University of South Carolina, Pediatrics) and Dr. Matthew Scott (Virginia Commonwealth University Health System, Internal Medicine/Pediatrics).
Our fellows have continued to participate in research in preschool asthma actively (Dr. Offerle; mentors Dr. Borish and Dr. Teague), alpha-gal allergy and its impact on heparin use (Dr. Nguyen; mentor Dr. Wilson), adult asthma phenotypes and novel treatments (Dr. Perozo; mentor Dr. Borish), and alpha-gal allergy related to biologic agents (Dr. Richards; mentors Dr. Wilson and Dr. Platts-Mills). They have presented their work at the American Academy of Asthma Allergy and Immunology (AAAAI) and American College of Asthma Allergy and Immunology (ACAAI) national meetings, as well as the annual Swineford Allergy Conference held on Grounds in April 2025. We commend our fellows for their academic scholarship and research achievements on top of a growing inpatient consultation service and busy outpatient clinics.
Our program administration saw a dramatic change this past year. We were excited to welcome a new Program Director. While new to the role, she was not new to our program. Dr. Samantha Minnicozzi took on the role of Program Director in July 2024, having previously served as APD. Dr. Minnicozzi is trained in Pediatrics. She completed her fellowship at Boston Children’s Hospital, where she completed cross-training in Adult Allergy and Immunology at Brigham and Women’s Hospital before joining the Department of Pediatrics in July 2019. She holds a dual appointment in the Department of Medicine and has been heavily involved in the education of our trainees since her arrival.
But announcing a new Program Director must mean our previous PD departed. Well, sort of: our Division was exceptionally proud to learn that Dr. Monica Lawrence was selected to be UVA’s next Designated Institutional Official (DIO) in April 2024, following the departure of Susan Kirk, MD. Having dedicated her career to the education of trainees, Dr. Lawrence continues to innovate and advocate for our trainees, now not just in our Division but across the institution and beyond. We were excited to have her continue this academic year as Associate Program Director. Again, congrats Monica!
And our Division is Growing

READ THE FULL MAY 2025 ISSUE OF MEDICINE MATTERS
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, In the Know, News and Notes, Notable Achievements, Publications, Research

