 Message from Amber Inofuentes MD, Hosptial Medicine Division Chief
Message from Amber Inofuentes MD, Hosptial Medicine Division Chief
2024 marked a momentous milestone for Hospital Medicine, which became the 11th division in the Department of Medicine on July 1st. The past year has been a time of tremendous growth and transition as we onboarded a record twelve new faculty and APP team members and built our new division administrative team. In addition to hiring several new graduates, including those from our residency program, we were fortunate to recruit several experienced hospitalist clinicians who decided to transition from community practice to an academic medical center. I hope you will take the time to read the included profiles of our many new colleagues and administrative staff.
We were fortunate to recruit Brigitte Binard as our division administrator, who had spent the prior year serving as associate division administrator for the Division of General Medicine, Geriatrics, Palliative and Hospital Medicine. Brigitte brings a wealth of experience in accounting, business operations, and management and has hit the ground running to develop and support our evolving strategic aims.
As we matured from section to division, our leadership team evolved to meet the unique needs of an academic hospitalist program. Andrew Parsons has become our director for research and academic advancement to support our expanding research and scholarship portfolio and oversee faculty promotion. Alex Millard has taken on the director of education and faculty development role to support ongoing medical education and professional development. George Hoke, who has served for several years as the director for faculty development, will continue to support hospital medicine in a newly created role directing recruitment and retention, focusing the latter on overseeing efforts to reduce or eliminate low-value tasks (often within the electronic health record) that occupy clinicians’ time, resulting in burnout and fatigue.
As the general medicine/hospitalist census continues to climb (averaging 140 patients last year, up over 40% from pre-COVID volumes), it was imperative to expand Ryan Wiggins’ role as director of clinical operations. I am incredibly proud that the hospitalist program has supported unprecedented patient volumes under his leadership despite last year’s staffing challenges through a model focused on adaptability and flexibility. This model allowed us to rarely utilize on-call backup physicians and avoid pulling hospitalists off teaching wards to manage volatile patient surges.
While expanding clinical volumes, we have continued to advance our strategic aims in clinical innovation and excellence, medical education, and faculty development. The newsletter will discuss highlights across these mission areas in more detail. Charlie Magee continues to lead an impressive interprofessional team that is dramatically reducing low-value cardiac monitoring; Omar Alsamman successfully partnered with clinical informaticists to implement an embedded AI tool to improve diagnosis capture and reduce coding query burden; Shri Gadrey is on the cusp of an R01 grant to support his groundbreaking respiratory kinematics research; and Andrew Parsons became an associate dean for the School of Medicine overseeing clinical education, to name of a few of our most significant achievements. Three more of our faculty (Usmaan Bashir, Jess Dreicer, and Greg Young) were also successfully promoted to associate professor.
In the clinical arena, our APP program onboarded two additional team members. It pivoted its model of care mid-year to become our Hospitalist East service in a collaborative practice model with our three North hospitalist physicians. In recognition of his diligent leadership of this program, his success as 3N acute medical director, and his multidisciplinary efforts to develop a limb preservation pathway, Rob Becker received one of this year’s Department of Medicine Awards for Clinical Excellence.
Looking into 2025, the division is excited to lead the way in developing clinical care pathways through an EMR-based tool, AgileMD; this tool allows us to improve the quality and consistency of disease-specific care while reducing frontline clinician frustration through embedded decision support. We also plan to build on last year’s quality improvement successes by partnering with medicine units to minimize delays between discharge orders and patient departure and by reducing low-value care while enhancing advanced care planning through structured use of the evidence-based surprise question.
Given ongoing pressures to expand clinical capacity, we are establishing clinical operations partnerships with our emergency medicine colleagues to improve patient care quality. We are also excited to support two new faculty participants in our Early Career Scholars program: Ben White will be working with Kyle Enfield, DOM vice chair for quality, to implement an evidence-based deprescribing program for anti-psychotic medications initiated during MICU hospitalizations, while Tareq Arar will be evaluating differences in clinical outcomes of patients admitted with heart failure to general medicine/hospitalist versus cardiology services.
As a group, we’d like to extend our gratitude to Cyndi Smith and Dr. Mohan Nadkarni, division administrator and chief for the division of General Medicine, Geriatrics, and Palliative, for their support during our transition, and to the rest of the Department of Medicine for its commitment to our success as a division.
We hope you will all stop by for a visit one day soon in our new space on the second floor of the West Complex, D wing.
~Amber Inofuentes MD
At left: Hospital Medicine Faculty
Back row left to right: Emily Richardson, Brian Peterson, Paul Helgerson, Cameron Webb, Charles Magee, Joseph Hall, Omar Alsamman, Andrew Parsons, Benjamin Sneed, Donald Molnar (Photo Kim Kelley-Wagner)

Front row left to right: Jessica Stevens, Kristin Long, Rahul Mehta, Ryan Wiggins, Amber Inofuentes, Jess Dreicer, Rebecca Kenner, Mary Hardy, Glenn Moulder, Anirudh Sundararaghavan, Shrirang Gadrey (Photo Kim Kelley-Wagner)
Research Updates
Novel Respiratory Monitoring System Gains Traction After Successful Proof-of-Concept
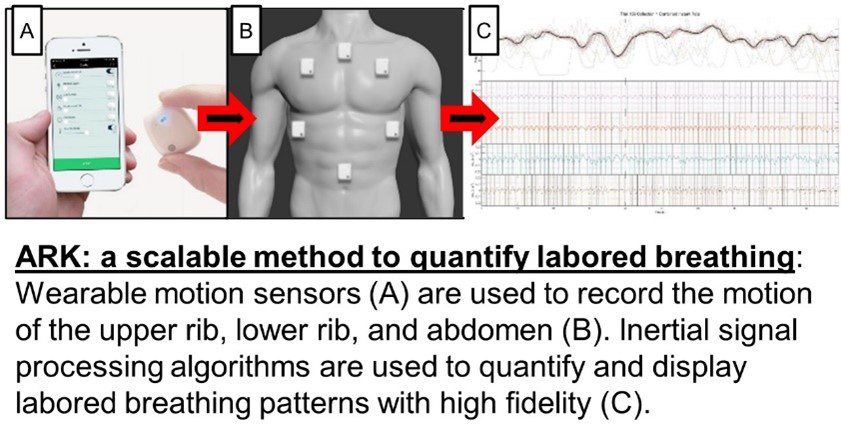 Dr. Shri Gadrey identified a critical flaw in contemporary patient monitoring systems – their inability to quantify high-risk labored breathing patterns. To address this gap, he led a multidisciplinary effort to develop a novel labored breathing monitor called ARK (Analysis of Respiratory Kinematics). This device uses inertial sensors to quantify breathing patterns (i.e., respiratory kinematics). In a proof-of-concept study of 108 hospital patients, ARK improved the prediction of critical illness beyond conventional predictors. This success was featured in a recent UVA Today article. Powered by their groundbreaking innovation, the ARK team is now poised to pioneer the large-scale measurement of human respiratory kinematics.
Dr. Shri Gadrey identified a critical flaw in contemporary patient monitoring systems – their inability to quantify high-risk labored breathing patterns. To address this gap, he led a multidisciplinary effort to develop a novel labored breathing monitor called ARK (Analysis of Respiratory Kinematics). This device uses inertial sensors to quantify breathing patterns (i.e., respiratory kinematics). In a proof-of-concept study of 108 hospital patients, ARK improved the prediction of critical illness beyond conventional predictors. This success was featured in a recent UVA Today article. Powered by their groundbreaking innovation, the ARK team is now poised to pioneer the large-scale measurement of human respiratory kinematics.
 NHLBI funding to study respiratory kinematics in the emergency room. Based on the feasibility and utility of ARK, Gadrey and team sought R01 funding from NHLBI. This proposal has received an enthusiastic response in the scientific review stage (8th percentile impact score) and now awaits the advisory council stage. If funded, this $4 million award will allow the ARK team to study respiratory kinematics in a prospective cohort of 1800 emergency room patients.
NHLBI funding to study respiratory kinematics in the emergency room. Based on the feasibility and utility of ARK, Gadrey and team sought R01 funding from NHLBI. This proposal has received an enthusiastic response in the scientific review stage (8th percentile impact score) and now awaits the advisory council stage. If funded, this $4 million award will allow the ARK team to study respiratory kinematics in a prospective cohort of 1800 emergency room patients.
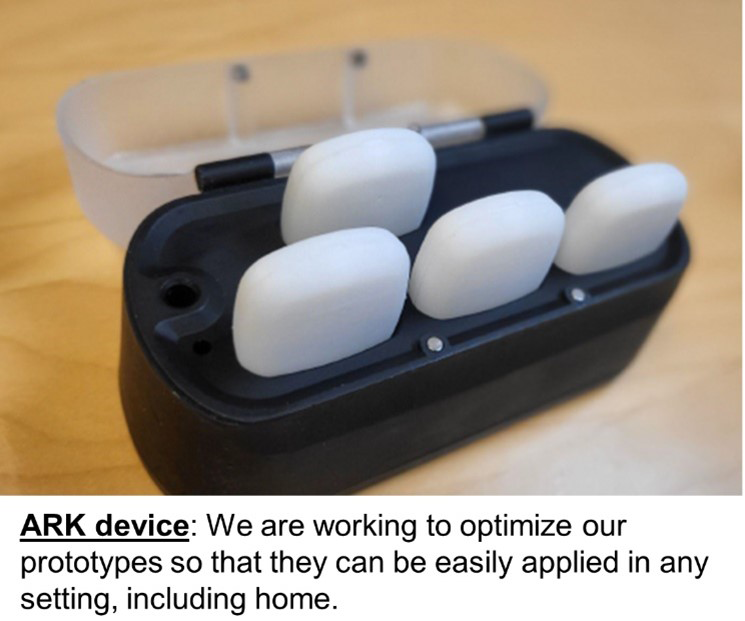
VIPC funding for home monitoring of respiratory kinematics in asthmatic children. The ARK system is simple enough to be applied in any setting, including homes. As such, home monitoring in asthmatic children is one of ARK’s highest-priority applications. The Virginia Innovation Partnership Corporation (VIPC) has awarded the ARK team $100,000 to optimize prototypes and create secure data pipelines for home monitoring in asthmatic children. The ARK team has partnered with UVA’s world-renowned pediatric asthma expert, Dr. Gerry Teague, to validate ARK in pediatric asthma.
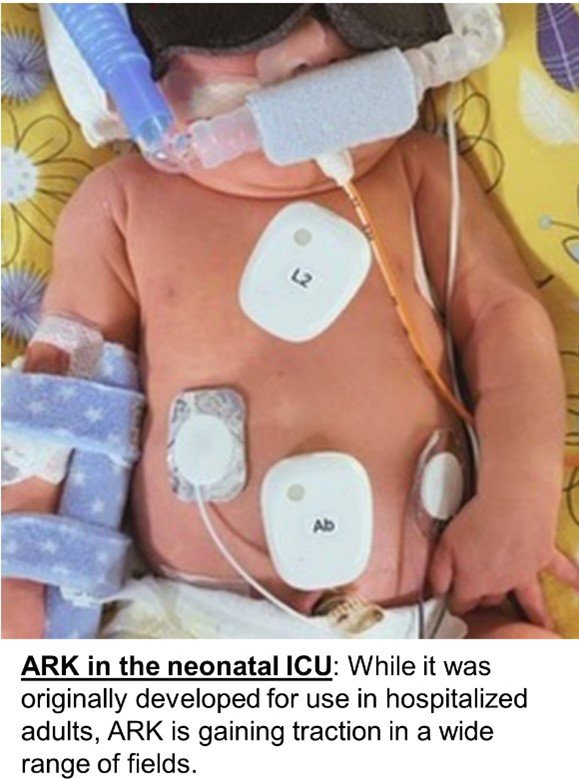 Ivy Foundation funding to study respiratory kinematics in premature neonates. Neonatal ICU infants are at high risk for respiratory failure, and breathing patterns (apnea, extreme periodic breathing) are known to herald respiratory deterioration. UVA neonatologist Dr. Brynne Sullivan has been awarded a $90,000 research grant by the Ivy Foundation to validate ARK in the NICU.
Ivy Foundation funding to study respiratory kinematics in premature neonates. Neonatal ICU infants are at high risk for respiratory failure, and breathing patterns (apnea, extreme periodic breathing) are known to herald respiratory deterioration. UVA neonatologist Dr. Brynne Sullivan has been awarded a $90,000 research grant by the Ivy Foundation to validate ARK in the NICU.
References:
1) Ashe WB, Innis SE, Shanno JN, Hochheimer CJ, Williams RD, Ratcliffe SJ, Moorman J R, & Gadrey SM (2022). Analysis of Respiratory Kinematics: A method to characterize breaths from motion signals. Physiological Measurement 43 015007.
2) Ashe WB, McNamara BD, Patel SM, Shanno JN, Innis SE, Hochheimer CJ, Barros AJ, Williams RD, Ratcliffe SJ, Moorman JR, Gadrey SM, Kinematic signature of high-risk labored breathing revealed by novel signal analysis, medRxiv 2023.06.08.23291170.
3) “Every Breath You Take: Invention Detects Breathing Problems Before It’s Too Late”
Quality Highlights
Improving Urine Testing Diagnostic Stewardship
by Amber Inofuentes MD
In 2023, UVA Hospital Medicine identified diagnostic stewardship as an important opportunity for improved quality of care on review of all instances of catheter-associated-urinary-tract infections (CAUTI) when hospitalist faculty were discharging attendings, an opportunity further supported by the CAUTI Coalition’s investigation of all hospital-wide CAUTI events that same year. As part of Hospital Medicine’s annual group quality projects, Dr. Rebecca Corey joined the CAUTI Coalition. She partnered with infectious disease physicians Drs. Patrick Jackson and Greg Madden to address urine testing diagnostic stewardship gaps. In addition to contributing to the inappropriate diagnosis of CAUTI, inappropriate urine testing (including in patients without an indwelling urinary catheter) contributes to inappropriate antibiotic prescribing, including treatment of asymptomatic bacteriuria or prescribing antibiotics for urinary tract infections (UTI) that are too broad in spectrum and/or too long in duration. Inappropriate antibiotic use can increase antibiotic resistance, length of hospital stay, and Clostridium difficile infections. UVA recently published institutional guidelines for evidence-based diagnosis and treatment of UTI that are inconsistently followed. Dr. Corey’s project aimed to reduce the inappropriate treatment of asymptomatic bacteriuria by reducing overall urinalysis orders (and, in turn, inappropriate urinalysis orders) through the application of the Plan-Do-Study-Act quality improvement method.
Dr. Corey’s team, which also included medical student Will Lain and QPI Coach Priya Ramayanam, performed data analysis of the current state by reviewing urinalysis and antibiotic ordering practices for UTI on three inpatient medicine acute care units (3 West, 3 Central, 3 East) to understand gaps between current practice and evidence-based guidelines. This analysis revealed that unnecessary urinalysis orders were the most significant opportunity. Across the preceding twelve months, appropriate indications for urinalysis orders were documented only 47% of the time. In 25% of those cases, patients lacking an appropriate indication for testing still received antibiotics, demonstrating that 13% of patients with urinalysis testing on these units received inappropriate antibiotics for asymptomatic bacteriuria. To identify the root causes of inappropriate testing, the team created a pareto chart of the most common reasons for inappropriate urinalysis orders. Three of the most frequent reasons identified were 1) isolated fever without urinary symptoms, 2) acute encephalopathy with other more likely etiology, and 3) diagnostic evaluation for noninfectious conditions such as acute kidney injury.
Based on these results, Dr. Corey’s team worked with the CAUTI Coalition to revise urinalysis orders in Epic by creating enhanced clinical decision support pathways. These orders provide prompts that nudge clinicians toward utilizing appropriate indications for urinalysis ordering for infectious and noninfectious indications and was published in Epic in late July. Her team’s work was presented as a poster in May at the 2nd Annual UVA Health QI/PS Showcase. This academic year, Hospital Medicine plans to evaluate the impact of these changes on urinalysis ordering habits to determine whether this important intervention has successfully reduced inappropriate testing and inappropriate antibiotic prescribing for asymptomatic bacteriuria.
Thanks to Dr. Andrew Barros for providing data analytics support to the team.
Telemetry Stewardship
by Charles Magee MD, 3 West medical director
Telemetry Stewardship took a giant step forward this past year in Hospital Medicine. As previously shared, our first telemetry stewardship Plan-Do-Study-Act (PDSA) cycle offered education and interdisciplinary communication on telemetry stewardship with a 44% reduction in telemetry time on 3West. Yet, the unit continued to experience instances where telemetry utilization exceeded the unit’s capacity. Therefore, a second PDSA cycle was commenced to improve stewardship by alerting our teams whenever telemetry orders exceeded recommended monitoring durations.
Based on the published alert model from NYC+ Health1, clinical informaticist Dr. David Ling helped design a Best Practice Advisory (BPA) according to order-specific indications. To improve engagement with the BPA, parameters were set to limit the BPA to fire only when providers enter the “Manage Orders” tab between 7 a.m. – 5 p.m. Alerts were blocked from firing for patients with a knowable telemetry indication, such as critical electrolyte derangements. We also wanted to provide teams time and space to make informed decisions, so we included a deferral option that snoozes the alert for 6 hours.
The BPA went live on 3West in November 2023 with an immediate reduction in telemetry usage that led nursing leadership to request its rapid deployment across all acute care general medicine starting in February 2024. This timely expansion freed up telemetry monitoring equipment for other clinical areas, deferring an institutional expense of nearly $245,000 for additional telemetry equipment.
Over the past ten months, the BPA has fired over 1,000 times, leading to an overall telemetry discontinuation rate of over 63%. The BPA does occasionally reach providers who indicate they are not the treating providers, although not often, just 92 times in total, and is usually alerting subspecialty fellows and consultants closely involved in the care of these patients. When removing these from the total, the BPA discontinuation rate for those making decisions about telemetry is above 69%! Teams also appreciate the option to defer a decision for six hours, frequently leading to termination with the next BPA or before the BPA can fire again. We also see interdisciplinary teams discussing telemetry in rounds, demonstrating a shared understanding of telemetry indications and stewardship focus. Most importantly, our preliminary analysis has shown no increases in escalation of care, evincing a lack of patient harm through active telemetry stewardship. Our units are notably quieter with less alarm fatigue, and a decreased nursing burden of patients requiring monitored transportation off unit.
A testament to the positive reception of the BPA, students, and residents have shared this work with leaders in other clinical areas, with exciting developments on the horizon. The acute stroke team from Neurology has embarked on a pathway to launch a similar BPA, and 4East has also voiced a clear interest in telemetry stewardship for their patient population.
This work has transformed how our teams perform telemetry stewardship toward a generation of high-value care. We offer our most sincere and heartfelt thanks to all our provider and nurse teams embracing telemetry stewardship into your everyday practice!
1. Krouss M, Israilov S, Alaiev D, et al. Tell-a provider about tele: Reducing telemetry overuse across ten hospitals in a safety net system. J Hosp Med. 2023;18(2):147-153. doi:10.1002/jhm.13030
Clinical Program Updates
Bridging the Gap Between Inpatient and Outpatient Opioid Use Disorder Treatment
by Drs. Alexandra Schwab and Rachel Kon
Despite clinicians’ best efforts to reduce narcotic prescriptions in the treatment of complex chronic pain, opioid-related deaths continue to rise. In response, in 2023, the federal government removed the X-waiver requirement for prescribing buprenorphine for opioid use disorder (OUD), coinciding with an all-time high in demand for substance use disorder (SUD) treatment in the Charlottesville area. UVA’s medicine residency program has recognized the needs of our local community and responded to changes in prescriber licensing by increasing both classroom education and bedside clinical experiences with a goal for all residents to develop the skills necessary to initiate and maintain patients on buprenorphine for OUD treatment upon graduation. To provide clinical training and meet patient demand for low-barrier OUD treatment in the primary care setting, we have started an OUD treatment program within our University Medical Associates (UMA) resident continuity clinic called UMA OBOT. This program welcomes our current patients to a specialized session on Monday afternoons with trained faculty, pharmacists, social workers, and an RN coordinator to provide comprehensive multidisciplinary care. Designed to bridge the gap between inpatient and outpatient medicine, patients with OUD who are ready to start treatment but do not have a PCP can be referred to UMA OBOT for both an outpatient prescriber and a new PCP.
Dr. Alexandra Schwab, a recent graduate of UVA’s residency program, and Dr. Rachel Kon, associate program director and director of PC track, have worked together for nearly twelve months to develop a clinic that will provide patients access to SUD treatment in a primary care office within a week of initial contact to the clinic. The clinic’s RN coordinator, Melissa Warren, facilitates seamless transitions and initial intake for the outpatient visit. Dr. Schwab has a unique role in the Department of Medicine, splitting time 50% as an outpatient provider, including her role providing addiction expertise and 50% performing clinical care in hospital medicine. This has allowed her to create therapeutic alliances with patients whom she admits for complicated withdrawals, drug detoxifications, or frequent readmissions for chronic pain. Treatment does not stop when the patient is discharged; she assists with coordinating follow-up and ongoing care in the outpatient setting. Her position includes resident education during clinic sessions and will soon include hospitalist education sessions during inpatient wards. As treatment for SUD evolves, general internists need to help meet the increased needs of patients with the necessary knowledge and skills for initiating and prescribing buprenorphine. We hope that offering OUD treatment will improve meaning and satisfaction of residents and faculty providing primary care for patients with chronic pain. We also hope that it will help reduce readmission rates for patients presenting with overdose-related complications or those seeking treatment options for chronic pain.
Please send questions or patient referrals to Alexandra Schwab, Melissa Warren, and Rachel Kon.
We have come a long way and look forward to more innovations in the months ahead.
Hospital Medicine Implements Admission and Throughput Coordinator RN
by Ryan Wiggins, director of clinical operations
Emilia Braun, BSN RN, joined the Hospital Medicine family as our inaugural admission and throughput (ATC) RN coordinator in December 2023. She brings a wealth of nursing experience, having worked in acute care medicine, cardiac cath lab, and infection prevention and control during her career at UVA Health. In her new role, she works closely with the patient placement center, emergency room, transfer center, and general medicine/hospitalist admitting teams to improve patient flow and progression. The timing of this role could not have been better, helping medicine accommodate our growing census and transfer volumes to better serve and care for patients in our local community and from all over the commonwealth.
Implementation of this role also facilitated incremental process redesign of admitting workflow for general medicine/hospitalist teams, eliminating previously redundant or low-value steps. As a result of these changes and additional hospital medicine efforts, last year, hospital medicine successfully reduced the median time from ATC consultation to admission orders by fifteen minutes (17%), providing timely evaluation and management of patients with an ever-increasing medical and social complexity.
Education Updates
Depth and Breadth of Hospitalist Teaching
by Alex Millard and Andrew Parsons
The Division of Hospital Medicine continues to make significant strides in medical education. In addition to providing exceptional clinical teaching in the General Medicine and Hospitalist Sub-I rotations, hospitalists are taking on pivotal roles within the School of Medicine. Our faculty members are deeply involved in the pre-clinical and clinical phases of undergraduate medical education (UME), positioning the Division as a key contributor to the foundational training of future physicians. Notably, hospitalists comprise the largest cohort of Foundations of Clinical Medicine coaches, playing an integral role in shaping medical students’ clinical skills and professionalism.
The Division’s impact extends beyond UME to graduate medical education (GME), where hospitalists are involved in multiple teaching capacities, contributing to the development of residents and fellows. Furthermore, with the successful growth of the Advanced Practice Provider (APP) service within Hospital Medicine, our group has expanded its reach to include teaching in the School of Nursing. This multifaceted involvement in education highlights the Division’s ongoing commitment to training the next generation of healthcare professionals, ensuring they have the skills and knowledge to excel in a rapidly evolving healthcare environment.
Clinical Education
Hospitalists attend 118 2-week blocks on General Medicine and had 29 month-long ACE rotators for the 2023-2024 year. The Hospitalist ACE remains one of the most in-demand ACE rotations at UVA due to the clinical rigor and direct clinical teaching and feedback students receive.
Undergraduate Medical Education
Launched in 2018, the Foundations of Clinical Medicine (FCM) program is a four-year curriculum focused on clinical skill development and professional identity formation. Within the UVA School of Medicine curriculum, morning lectures primarily concern basic science knowledge. The practice of medicine—both the science and the art in all its subtleties—is the focus of FCM. Physician coaches lead FCM. Hospitalists comprise 30% of all FCM coaches: Ian Crane, Charlie Magee, Rahul Mehta, Glenn Moulder, Chris Moore, Andrew Parsons, Ben Sneed, and Greg Young are regular coaches. Greg Young is the FCM Phase 2/3 course director. Alex Lawson and Brian Peterson are part of the Coach Associates Faculty Development Program.
Cameron Webb is the Bedside to community course director and Public health and health policy thread leader for medical students.
Amber Inofuentes is the patient safety and quality thread leader for medical students. The Intersessions Course began in March 2021 and is co-directed by Dr. Greg Young. This multidisciplinary course consists of 3 one-week sessions paired with each trimester of a student’s clerkship year. The threefold main goals objectives of the course are for students to (1) integrate learning experiences to enhance clinical learning through activities designed to revisit basic science, incorporate curricular threads, and practice clinical skills such as physical exam techniques, diagnostic reasoning, quality improvement, communication, and other clerkship-specific procedures and skills; (2) explore and expand personal career interests with exposure to areas of clinical medicine not currently included in the clerkship year; and (3) meet with their Foundations of Clinical Medicine (FCM) coaches to review clinical performance data and create individualized learning plans.
Alex Millard and Glenn Moulder are co-associate clerkship directors for the IM phase 2 clerkship. During this rotation, nine hospitalists contributed to the Clinical Skills Education Program (CSEP), where clerkship students are taken weekly to practice the evidence-based physical exam focused on cardiac, pulmonary, and abdominal exams.
Brian Peterson is co-director for the Acute Care and Internal Medicine track for the Internship Readiness Course, a two-week required course around Match Day. Students choose between specialty tracks, including surgery, pediatrics, acute care, internal medicine, obstetrics and gynecology, and pathology. This course increases students’ readiness for residency by reviewing necessary clinical knowledge and skills. The course incorporates case-based and small-group sessions, hands-on procedural training, and simulation. In 2024, eighteen hospitalists contributed to the course for 187 teaching hours.
Ian Crane, Andrew Parsons, and Greg Young are UME specialty remediation coaches. In addition to George Hoke, those three are Clinical Mastery Elective Directors, aiding students needing additional clinical instruction every year.
Rahul Mehta is the MSTP clinical skills workshop leader and directs the popular Consultative and Perioperative Medicine elective.
Charlie Magee and Glenn Moulder act as faculty mentors for the Choosing Wisely STARS program for medical students, supporting student-led initiatives to improve high-value care.
Graduate Medical Education
Rebecca Clemo, Jess Dreicer, and Alex Millard are associate program directors for the IM Residency Program. Rebecca Clemo focuses on clinical reasoning and cognitive bias, helping with resident M&M. Jess Dreicer leads the residency program’s quality improvement and patient safety curriculum and oversees mentorship for resident QI projects. Alex Millard focuses on evaluation and assessment with the residency program.
Ian Crane, Alex Millard, Glenn Moulder, Rudi Sundararaghavan, Andrew Parsons, and Cameron Webb are core mentors for residents, helping them develop individual learning plans and aiding in career direction over their three years in residency.
Glenn Moulder and Emily Richardson teach in the residency +1 curriculum, focusing on high-value care.
Additionally, hospitalists contribute to both IM residents and orthopedic surgery and rotating residents on the Consultative and Perioperative Medicine rotation, for which Rahul Mehta is the elective director.
Other Teaching Activities
Numerous hospitalist faculty are members of the SOM-wide Academy for Excellence in Education, including Ian Crane, Jess Dreicer, Ben Martin, Rahul Mehta, Alex Millard, Glenn Moulder, Andrew Parsons, Brain Peterson, and Greg Young.
Rob Becker, Mary Hardy, ACNP, Deb Okyere, AG-ACNP, and Conner Lawrence, AG-ACNP, have all worked as preceptors for the School of Nursing ACNP capstone and clinical.
Practicum students. Despite being launched only one year ago, the Hospital Medicine APP service is a frequently requested practicum experience for nurse practitioner students due to the acuity, complexity, and range of diagnoses hospital medicine cares for.
George Hoke is the co-instructor of the post-bac pre-medicine program at the School of Continuing Education.
Cameron Webb teaches in the Batten School with courses on Introduction to Health Policy and Crisis Policymaking.
Ben Martin is the assistant director of programs in Health Humanities at UVA’s Center for Health Humanities and Ethics and teaches a two-week phase 3 elective in “Literature and Medicine” and “Calls of Medicine.” He is also the director of the Edward Hook Scholarship Program in Biomedical Ethics and Humanities.
Andrew S. Parsons, MD, MPH, Announced Associate Dean for Clinical Competency
Andrew Parsons, MD, MPH, associate professor of medicine, took on the role of associate dean for clinical competency in the School of Medicine (SOM) starting July 2024. Dr. Parsons oversees the SOM’s longitudinal clinical skills and competency-based educational programs in his new role. These include the Foundations of Clinical Medicine curriculum and course directors, the FCM Coaching Program and Coaching Associates Program, the Entrustable Professional Activities (EPA) Program, Designated Assessors, the Entrustment Committee, and the EPA Leadership Group. He leads the Observed Structured Clinical Examination (OSCE) assessment program and the Clinical Remediation Program. He oversees the Clinical Performance Education Center (CPEC), including the Simulation Center, the Clinical Skills Center, and the Surgical Skills Training Center, working with the directors of each center to ensure appropriate utilization, standardization, integration, and innovation of these critical resources within the curriculum. Dr. Parsons is an accomplished educator and scholar who is a national leader in clinical skills education. He is pursuing his PhD in Health Professions Education at Maastricht University in the Netherlands, where his research focuses on clinical reasoning in education and clinical practice. Dr. Parsons also leads UVA’s Clinical Reasoning Research Collaborative (CRRC), a physician research group aiming to improve reasoning education and positively impact patient care.
Ian Crane, MD, Continues a Successful Research Program in Pre-Rounding Practices
Ian Crane, MD, is exploring the pre-rounding practices of experienced hospitalists to guide interventions and support programs for learners, including those who struggle with organization and efficiency in the clinical environment. His efforts involve the creation of highly realistic patient charts in a simulated electronic health record paired with a key-features-based clinical reasoning assessment and a pre-rounding methodology assessment. Dr. Crane’s research employs Cognitive Task Analysis (CTA) and direct observation to outline expert pre-rounding techniques. His early work was funded by the Division of Hospital Medicine’s Early Career Scholars (ECS) Program, and more recently, he was awarded a research grant by the Center for Excellence in Education (CEE). He has presented this work at the national AAIM conference and UVA Med-Ed Lecture Series. He was recently selected to the CEE Scholars Program to continue this work with formalized training and mentorship.
Honors and Awards
Amber Inofuentes MD – UVA School of Medicine Dean’s Award for Clinical Excellence
Andrew Parsons MD – Alpha Omega Alpha (AOA) Honor Society Faculty Inductee
Brain Peterson MD – Most Outstanding Presentation Award from UVA School of Medicine Innovations in Education Week
Robert Becker MD – Department of Medicine Award for Clinical Excellence
Christopher Moore MD – Department of Medicine Award for Excellence in Education
Ian Crane MD – Department of Medicine Award for Excellence in Education
Ian Crane MD and Ben Martin MD received the School of Medicine Excellence in Performance Assessment Award for providing quality and quantity of feedback in Entrustable Professional Activities for medical students.
Ben White MD and Tareq Arar MBBS were selected for the Division’s Early Career Scholars Program.
Ian Crane MD and Brian Peterson were selected into the School of Medicine’s Center for Excellence in Education Scholars Program.
Read the full November 2024 issue of Medicine Matters.
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, In the Know, News and Notes, Notable Achievements, Publications, Research, Top News
