Message from Michael Nelson MD PhD, Division Chief Asthma, Allergy & Immunology
 As the end of another academic year approaches, I look back over the excitement of the past year and the promise that lies ahead. Highlights of the past year are again plentiful.
As the end of another academic year approaches, I look back over the excitement of the past year and the promise that lies ahead. Highlights of the past year are again plentiful.
As many of you are already aware, Dr. Monica Lawrence was named the University of Virginia’s Designated Institutional Official overseeing all graduate medical education for the University following the departure and distinguished tenure of Dr. Susan Kirk. This is a tremendous, bittersweet honor for the Division as she transitions from fellowship director and some of her clinical and research duties. UVA GME is in great hands. Our fellowship will also be in great hands with Dr. Sam Minnicozzi, who will begin as program director this summer. UVA Medical Scientist Training Program (MSTP) program is also in great hands- congratulations to Professor Judith Woodfolk from our Division, who was recently named as an incoming co-director of this prestigious program, preparing the next generation of MD/PhD physician-scientists.
On the research front, the Platts-Mills and Wilson labs continued their work on the R37 and new supplement, contributing to groundbreaking research in alpha-gal hypersensitivity, including uncovering novel cardiovascular risks and striking regional epidemiology of alpha-gal sensitization in national military recruits. Did I mention that Dr. Platts-Mills was also awarded the prestigious 2024 Distinguished Scientist Award for career achievements from the American Academy of Allergy, Asthma and Immunology? The Borish lab continues its cutting-edge research in asthma pathogenesis, including leading a clinical trial studying viral-induced asthma pathogenesis and the impact of dupilumab. The Woodfolk lab is publishing its seminal work on distinct Type 1 immune networks underlying restrictive lung disease after COVID-19. The McGowan lab embarked on an RO1 studying eosinophilic esophagitis pathogenesis, epidemiology, and noninvasive testing. At a recent Gordon Conference, Charlene Dunaway Altamirano (2nd-year fellow) and mentors presented novel findings on Honduran children’s food allergen sensitization.
Not to be outdone on the clinical front, we are excited about expanding our services to the south by establishing a new outreach clinic in Lynchburg this summer led by Dr. Kyin. We are also completing our first year with a dedicated clinical immunology consult service triaged behind every consult to our inpatient general allergy-immunology consult service.
This year, we also marked another successful fellowship match for our training program. We matched our top two choices again this year. We welcome Amelia Perozo from Danbury, CT, and welcome back Nathan Richards, whom Dr. Wilson and Dr. Platts-Mills mentored as a research assistant before residency. Nathan now returns as a fellow in our program. How’s that for yet another example of outstanding mentorship in the Division?!
On April 12th and 13th, we hosted the 62nd Swineford Conference, marking Dr. Platts-Mills’ 40th edition of this clinical and scientific meeting. International and national experts contributed to the long tradition of cutting-edge science and clinical presentations, enabling the engagement of the entire audience in lively discussions. Invited distinguished extramural speakers included Professors Elizabeth Matsui (University of Texas at Austin), Paul Turner (Imperial College, London), Francesca Levi-Schaffer (Hebrew University of Jerusalem), Andrew Wang (Yale), Brian Vickery (Emory), Melody Carter (NIH), Martin Chapman (Inbio/Indoor Biotechnologies), Michael Blaiss (Medical College of Georgia) and Larry Schwartz (VCU).
I am eternally grateful to have received the Walter Reed Distinguished Achievement Award at SOM reunions last month. I am humbled to be on a list of recipients of this outstanding award, including such institutional pillars as Munsey Wheby, MD, Vivian Pinn, MD, Charles Gross, MD, and William Petri, MD, PhD. I am most appreciative to this institution, Carl Creutz, PhD (Pharmacology), Maurice Apprey, PhD (Psychiatry), Moses Woode, MD, DMED (Diversity Programs). Additionally, I’d like to thank my many other UVA mentors along the way who gave me my start in medicine and inspired me to return to UVA to continue to carry the torch handed to me by my mentors for the next generation of academic leaders. The future remains bright!
~ Michael Nelson MD PhD
Research Update
Borish Lab
 The Larry Borish, MD laboratory’s primary focus remains the role of rhinovirus (RV) in precipitating asthma exacerbations. These NIH-funded studies are designed to define the role of innate immune responses, including anti-viral and T2-promoting immune responses, by infected airway epithelial cells as they might distinguish the consequences of RV infections in asthmatics, allergic rhinitis, and healthy control subjects. For the next two years, the Borish laboratory will be the co-lead sponsor of a Regeneron-funded, investigator-initiated study entitled “Viral infection in asthma (VIA) Study.” This randomized, placebo-controlled study assesses cellular and molecular markers related to experimental RV infection in asthmatics and the effect of dupilumab in preventing exacerbations in this investigational model. This study will aim to assess the molecular and cellular basis by which dupilumab prevents the development of an RV-induced asthma exacerbation. Unrelated to the RV studies, the Borish lab collaborates closely with Dr. Gerry Teague in pediatrics as co-PI for studies addressing the role of mast cells and mononuclear phagocytic cells in the immune response to viral respiratory infections in children and adolescents with problematic wheeze. Additional NIH-funded studies have identified an immune deficit state in the airways of many infants with a persistent wheeze that leads to susceptibility to persistent RV injection, chronic neutrophilic bronchia alveolitis, and increased susceptibility to the development of asthma. We are enrolling patients in a Regeneron-sponsored study to demonstrate the ability of dupilumab to attenuate staphylococcus aureus infection in chronic sinusitis and ameliorate the dysbiotic state, including with restoration of a healthier antimicrobial state, including restoration of a healthier antimicrobial state.
The Larry Borish, MD laboratory’s primary focus remains the role of rhinovirus (RV) in precipitating asthma exacerbations. These NIH-funded studies are designed to define the role of innate immune responses, including anti-viral and T2-promoting immune responses, by infected airway epithelial cells as they might distinguish the consequences of RV infections in asthmatics, allergic rhinitis, and healthy control subjects. For the next two years, the Borish laboratory will be the co-lead sponsor of a Regeneron-funded, investigator-initiated study entitled “Viral infection in asthma (VIA) Study.” This randomized, placebo-controlled study assesses cellular and molecular markers related to experimental RV infection in asthmatics and the effect of dupilumab in preventing exacerbations in this investigational model. This study will aim to assess the molecular and cellular basis by which dupilumab prevents the development of an RV-induced asthma exacerbation. Unrelated to the RV studies, the Borish lab collaborates closely with Dr. Gerry Teague in pediatrics as co-PI for studies addressing the role of mast cells and mononuclear phagocytic cells in the immune response to viral respiratory infections in children and adolescents with problematic wheeze. Additional NIH-funded studies have identified an immune deficit state in the airways of many infants with a persistent wheeze that leads to susceptibility to persistent RV injection, chronic neutrophilic bronchia alveolitis, and increased susceptibility to the development of asthma. We are enrolling patients in a Regeneron-sponsored study to demonstrate the ability of dupilumab to attenuate staphylococcus aureus infection in chronic sinusitis and ameliorate the dysbiotic state, including with restoration of a healthier antimicrobial state, including restoration of a healthier antimicrobial state.
McGowan Lab
 Dr. McGowan’s group continues to expand their research on eosinophilic esophagitis (EoE), an emerging form of food allergy. Through her NIH/NIAID K23 Award, Dr. McGowan established the University of Virginia EoE Cohort with her collaborators, Drs. Bryan Sauer (Adult Gastroenterology) and Barrett Barnes (Pediatric Gastroenterology). This cohort longitudinally follows over 350 patients with EoE and has been used to examine immunologic drivers of this disease. In particular, her team found that immunoglobulin G4 (IgG4) may play an essential role in the inflammatory response in EoE. Through an NIH/NIAID R01 Award, they are examining whether this could be used to help identify food triggers in EoE patients. This work is being performed in collaboration with the laboratories of Dr. Judith Woodfolk (Allergy/Immunology) and Sarah Ewald (Microbiology). Dr. McGowan’s group also examined the epidemiology of EoE and found that children who live farther away from a pediatric gastroenterologist and those who live in more impoverished areas are less likely to be diagnosed with EoE. In addition, they found that EoE is often underdiagnosed among patients with other allergic conditions. This work has been funded by the American College of Gastroenterology (PIs McGowan and Sauer), iTHRIV, and the NIH/NIAID (K23, R21, R01). Last year, Dr. McGowan’s group expanded to include Rebecca Revell, a clinical research coordinator, and Dr. Roopesh Singh, a research scientist.
Dr. McGowan’s group continues to expand their research on eosinophilic esophagitis (EoE), an emerging form of food allergy. Through her NIH/NIAID K23 Award, Dr. McGowan established the University of Virginia EoE Cohort with her collaborators, Drs. Bryan Sauer (Adult Gastroenterology) and Barrett Barnes (Pediatric Gastroenterology). This cohort longitudinally follows over 350 patients with EoE and has been used to examine immunologic drivers of this disease. In particular, her team found that immunoglobulin G4 (IgG4) may play an essential role in the inflammatory response in EoE. Through an NIH/NIAID R01 Award, they are examining whether this could be used to help identify food triggers in EoE patients. This work is being performed in collaboration with the laboratories of Dr. Judith Woodfolk (Allergy/Immunology) and Sarah Ewald (Microbiology). Dr. McGowan’s group also examined the epidemiology of EoE and found that children who live farther away from a pediatric gastroenterologist and those who live in more impoverished areas are less likely to be diagnosed with EoE. In addition, they found that EoE is often underdiagnosed among patients with other allergic conditions. This work has been funded by the American College of Gastroenterology (PIs McGowan and Sauer), iTHRIV, and the NIH/NIAID (K23, R21, R01). Last year, Dr. McGowan’s group expanded to include Rebecca Revell, a clinical research coordinator, and Dr. Roopesh Singh, a research scientist.
Platts-Mills Lab
 The Platts-Mills’ lab is long-standing interested in understanding environmental and immunologic contributions to allergic disease. A major focus of the lab has been related to understanding how dust mites and cat allergens are causally related to asthma. More recently, our lab has been a primary driver in understanding a novel form of allergic reaction to red meat (alpha-gal syndrome or AGS) caused by tick bites. In 2018, we published a paper on the relationship between sIgE and alpha-gal, and evidence of coronary artery disease (CAD) samples were obtained by Angela Taylor, MD (UVA Heart and Vascular Center) using intravascular ultrasound (IVUS). In 2022, a major cardiology group in Sydney, Australia, confirmed our results on the positive association between alpha-gal and CAD. Most recently, we saw a woman in her 40s who had been seen initially 8-10 years prior for a severe episode of anaphylaxis and diagnosed with AGS. Just before her recent visit, she had two myocardial infarctions and now has five stents in her main cardiac arteries. Between her initial visit and these cardiac events, she maintained a strict diet, avoiding mammalian meat and organs; however, she continued to consume dairy products derived from Bos domesticus.
The Platts-Mills’ lab is long-standing interested in understanding environmental and immunologic contributions to allergic disease. A major focus of the lab has been related to understanding how dust mites and cat allergens are causally related to asthma. More recently, our lab has been a primary driver in understanding a novel form of allergic reaction to red meat (alpha-gal syndrome or AGS) caused by tick bites. In 2018, we published a paper on the relationship between sIgE and alpha-gal, and evidence of coronary artery disease (CAD) samples were obtained by Angela Taylor, MD (UVA Heart and Vascular Center) using intravascular ultrasound (IVUS). In 2022, a major cardiology group in Sydney, Australia, confirmed our results on the positive association between alpha-gal and CAD. Most recently, we saw a woman in her 40s who had been seen initially 8-10 years prior for a severe episode of anaphylaxis and diagnosed with AGS. Just before her recent visit, she had two myocardial infarctions and now has five stents in her main cardiac arteries. Between her initial visit and these cardiac events, she maintained a strict diet, avoiding mammalian meat and organs; however, she continued to consume dairy products derived from Bos domesticus.
Cases like this emphasize two questions: Should all patients or subjects with sIgE to alpha-gal be advised to avoid all mammalian products because of the potential chronic risk of cardiac disease (CAD)? This would include avoiding dairy products even though, in most cases, the products would not give rise to clinically apparent allergic reactions.
The most promising candidate for another marker is antibodies to alpha-gal of the IgG3 isotype. IgG3 is an inflammatory immunoglobulin that has recently been reported to ‘increase after implantation of porcine or bovine aortic valves.’ We are currently adapting the ImmunoCap 250 machine to assay IgG3-specific antibodies using reagents provided by Dr. Robert Moverare from Phadia Thermo-Fisher in Sweden.
Studies on TH2 antibody responses and Asthma
We have recently conducted detailed studies on specific IgE and IgG4 antibodies to component allergens (single proteins) of cat and dust mites in sera from six hundred teenagers participating in the Viva birth cohort in Boston. The primary evidence on these children shows that dust mites and cats are the main sources of asthma-related indoor allergens. However, analysis of the data on the two major allergens Der p 1 and Fel d 1 has revealed a striking difference in IgG4 compared to the responses to more recently identified allergens such as Der p 23, Fel d 4, and Fel d 7. As expected, the primary contributor to specific IgG4 for cat allergens was Fel d 1. However, the surprise is that the other cat allergens show no significant effect on sIgG4 related to living in a home with a cat. The most likely relevant feature of these secondary allergens is that they are present in extracts in significantly lower quantities. The results imply that IgG4 responses require a higher quantitative exposure than IgE responses. In addition, the results suggest that some of the allergens other than Der p 1 and Fel d 1 have greater relevance to asthma because they induce less IgG4 relative to IgE antibodies.
Wilson Lab
 Dr. Jeffrey Wilson’s primary clinical and research focus is on alpha-gal syndrome. Working with Dr. Platts-Mills and colleagues, his lab has been involved in studies better to understand alpha-gal epidemiology locally and across the USA. This work involved a UVA employee cohort recruited to study COVID-19 vaccine antibody responses and a DoD-funded project of 3000 military recruits collaborating with Dr. Cade Nylund at the Uniformed Services University of the Health Sciences. The lab also studies links between tick bites and alpha-gal sensitization and was awarded an NIH grant to recruit and follow individuals who have had recent tick bites. Based on a prior observation that alpha-gal sensitization was associated with heart disease, the lab has been involved with the NHLBI-sponsored Multi-Ethnic Study of Atherosclerosis. The goal has been to understand better whether IgE sensitization to alpha-gal is a risk factor for early coronary artery disease development. As part of these investigations, Dr. Wilson has ongoing collaborations with Dr. Coleen McNamara (Cardiology/Beirne Carter Immunology Center) and Prof. Loren Erickson (Microbiology/Beirne Carter Immunology Center). In partnership with Corinne A. Keet, MD, PhD at the University of North Carolina, the lab is also studying whether IgE sensitization to more common food allergens could contribute to cardiovascular disease.
Dr. Jeffrey Wilson’s primary clinical and research focus is on alpha-gal syndrome. Working with Dr. Platts-Mills and colleagues, his lab has been involved in studies better to understand alpha-gal epidemiology locally and across the USA. This work involved a UVA employee cohort recruited to study COVID-19 vaccine antibody responses and a DoD-funded project of 3000 military recruits collaborating with Dr. Cade Nylund at the Uniformed Services University of the Health Sciences. The lab also studies links between tick bites and alpha-gal sensitization and was awarded an NIH grant to recruit and follow individuals who have had recent tick bites. Based on a prior observation that alpha-gal sensitization was associated with heart disease, the lab has been involved with the NHLBI-sponsored Multi-Ethnic Study of Atherosclerosis. The goal has been to understand better whether IgE sensitization to alpha-gal is a risk factor for early coronary artery disease development. As part of these investigations, Dr. Wilson has ongoing collaborations with Dr. Coleen McNamara (Cardiology/Beirne Carter Immunology Center) and Prof. Loren Erickson (Microbiology/Beirne Carter Immunology Center). In partnership with Corinne A. Keet, MD, PhD at the University of North Carolina, the lab is also studying whether IgE sensitization to more common food allergens could contribute to cardiovascular disease.
Fellowship/Trainees Update
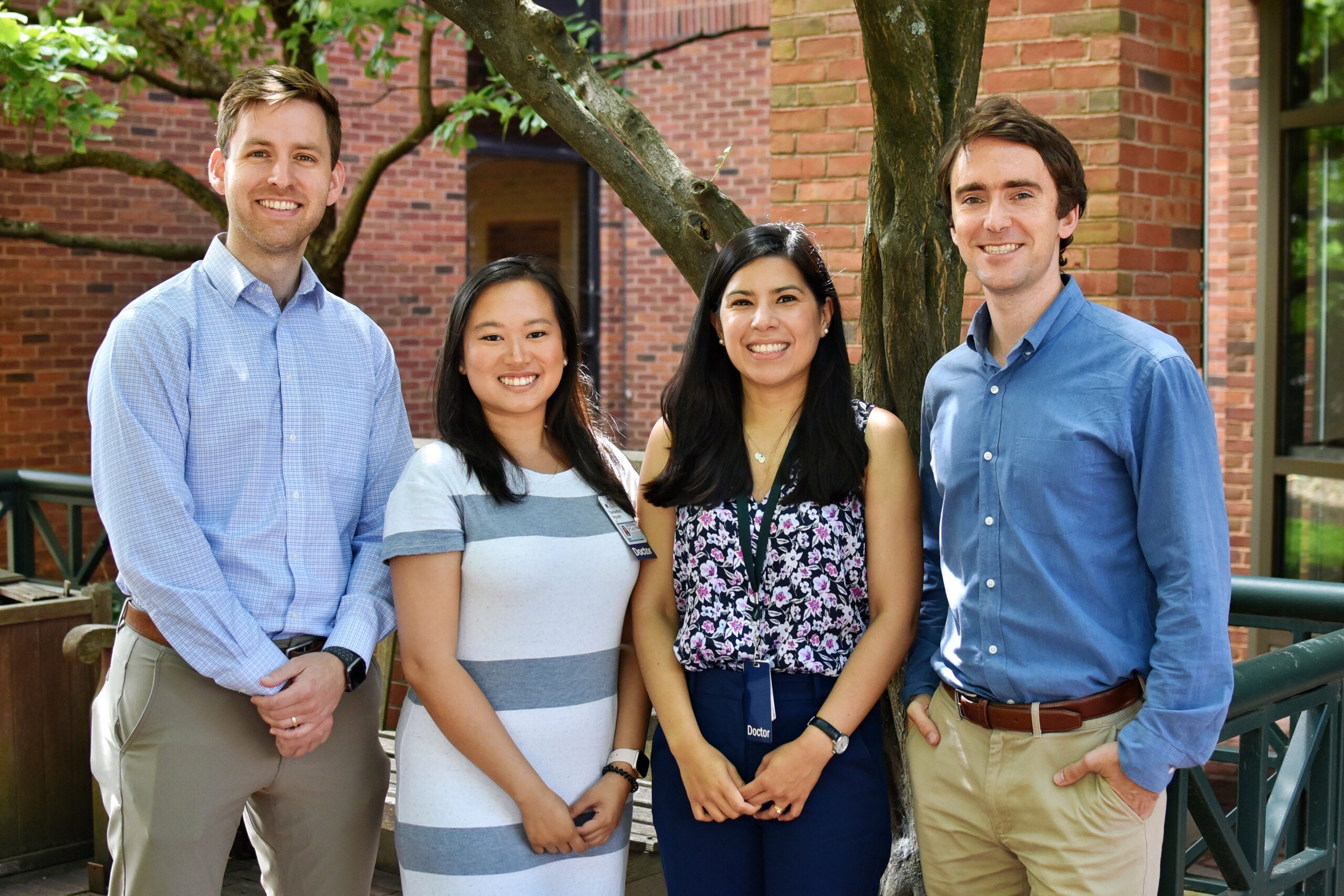
From left: Thomas Offerle, Samantha Nguyen, Charlene Dunaway Altamirano, and Marc Breidenbaugh
Our long-standing fellowship program continues to celebrate the many achievements of our fellows-in-training. We congratulate our 2024 graduating fellows, Dr. Marc Breidenbaugh, who will be joining Richmond Allergy & Asthma in Richmond, Virginia, and Dr. Charlene Dunaway Altamirano, who will remain on the Immunology Training Grant following the completion of her fellowship and then be joining the faculty here!
In July 2023, we welcomed two new fellows into the program: Dr. Thomas Offerle (Emory University, Pediatrics) and Dr. Samantha Nguyen (Wake Forest University, Internal Medicine). We also completed another very successful virtual recruitment season and are excited to welcome two new incoming fellows in July 2024: Dr. Amelia Perozo (Danbury Hospital, Internal Medicine) and Dr. Nathan Richards (Harnett Health, Internal Medicine).
Our fellows have continued to actively participate in research projects on the prevalence of food allergy in Honduras (Dr. Dunaway Altamirano; mentors Dr. Nelson, Dr. Platts-Mills, and Dr. Wilson), anxiety in pediatric food allergic patients (Dr. Breidenbaugh; mentor Dr. McGowan), preschool asthma (Dr. Offerle; mentors Dr. Borish and Dr. Teague), and eosinophilic esophagitis (Dr. Nguyen; mentor Dr. McGowan). They have presented their work at the American Academy of Asthma Allergy & Immunology (AAAAI) and American College of Asthma Allergy & Immunology (ACAAI) national meetings, as well as the annual Swineford Allergy Conference held on Grounds in April 2024. We commend our fellows for their academic scholarship and research achievements on top of a growing inpatient consultation service and busy outpatient clinics.
Accolades
 Following an extensive national search, UVA Health University Medical Center has selected Dr. Monica Lawrence as the Designated Institutional Official (DIO) and Associate Dean for Graduate Medical Education (GME), effective April 8. In this role, Dr. Lawrence will supervise all GME programs and approximately 850 residents, fellows, and trainees across our organization.
Following an extensive national search, UVA Health University Medical Center has selected Dr. Monica Lawrence as the Designated Institutional Official (DIO) and Associate Dean for Graduate Medical Education (GME), effective April 8. In this role, Dr. Lawrence will supervise all GME programs and approximately 850 residents, fellows, and trainees across our organization.
Dr. Judith Woodfolk was appointed to the NIH Immunity and Host Defense (IHD) Study Section in 2023 for a 3-year term and served as Co-Chair in 2024.
Dr. Glenda Canderan was appointed to the position of Research Assistant Professor of Medicine.
Naomi Bryant, a fifth-year graduate student, presented a poster at the 2024 AAAAI meeting entitled “Deep T-Cell Profiling Implicates Lung-Resident Rhinovirus-Specific Cells in the Development and Persistence of Severe Childhood Asthma.”
Paul Dell was selected for the 2024 American Academy of Allergy, Asthma, and Immunology (AAAAI) Cells and Mediators of Allergic Inflammation (CMAI) mentorship program. This program pairs participants with a basic scientist in their field for a variety of mentorship activities.
Drs. Glenda Canderan and Lyndsey Muehling attended the 2023 Biomedical Data Science Innovation Lab with the theme of “Data Science and the Public Health Consequences of the COVID-19 Pandemic”
Dr. Lyndsey Muehling presented a poster at the joint Innate Immunity and Systems Immunology Keystone Meeting.
Dr. Thomas Platts-Mills, was unanimously named as the 2024 recipient of the AAAAI Distinguished Scientist Award by The American Academy of Allergy, Asthma and Immunology.
Dr. Michael Nelson, was named the 2023 recipient of the Walter Reed Distinguished Achievement Award.
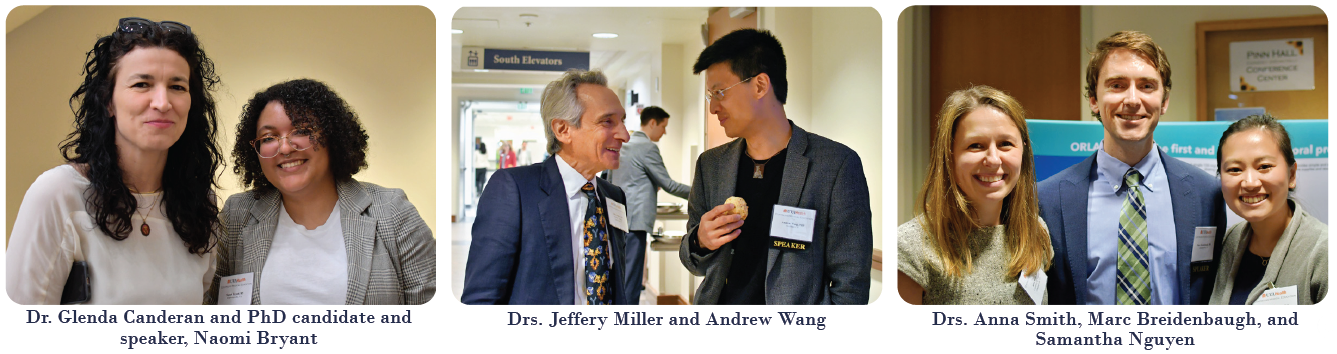
2024 62nd Swineford Allergy Conference – April 12th, 13th
 By Monte Parsons and Rebecca Jewell, Meeting Planning Committee
By Monte Parsons and Rebecca Jewell, Meeting Planning Committee
Pinn Hall once again hosted the prestigious Annual Swineford Allergy Conference, a testament to its status as the longest-running local Allergy meeting in the United States and one of the longest-running CME events in Virginia. This conference, proudly hosted by our Division, serves as a scientific gathering dedicated to educating physicians caring for patients with allergic disorders and for the scientists who work with them to develop a novel understanding of and treatments for allergic disease.
 Nearly one hundred speakers and participants gathered for this in-person meeting, and we were excited to welcome to the University of Virginia and to Charlottesville experts in our field who traveled from great distances (despite many travel-related hurdles) to share their knowledge and insight. Upholding the tradition of having international meeting faculty, this year’s speakers included Professor Paul Turner of the National Heart and Lung Institute, Imperial College (London UK), and Francesca Levi-Schaffer, PhD, from The Hebrew University of Jerusalem.
Nearly one hundred speakers and participants gathered for this in-person meeting, and we were excited to welcome to the University of Virginia and to Charlottesville experts in our field who traveled from great distances (despite many travel-related hurdles) to share their knowledge and insight. Upholding the tradition of having international meeting faculty, this year’s speakers included Professor Paul Turner of the National Heart and Lung Institute, Imperial College (London UK), and Francesca Levi-Schaffer, PhD, from The Hebrew University of Jerusalem.
Not to be outdone, our speakers from within the US came from all four points of the compass:
• North (Dr. Andrew Yang from Yale and Dr. Melody Carter from the NIH)
• West (Dr. Elizabeth Matsui from the University of Texas at Austin)
• South (Dr. Brian Vickery from Emory University and Dr. Michael Blaiss from Medical College of Georgia)
• East (Dr. Larry Schwartz from Virginia Commonwealth University)
The list of speakers highlighted includes those from Charlottesville: Marc Breidenbaugh, MD, and Charlene Dunaway Altamirano, MD, PhD (our outstanding second-year fellows), Naomi Bryant (PhD candidate in Dr. Woodfolk’s lab), and Dr. Martin Chapman (former UVA faculty member, Founder, and CEO of InBio, Inc.).
In keeping with this meeting’s traditions, there were excellent discussions of multiple topics, including the future of biologics in asthma, genetic testing for inborn errors of immunity, the study of antibodies to PEG, and the importance of lipids in maintaining the protective role of infant skin.
We have already started to plan for next year’s edition, our 63rd Swineford, which will take place in April 2025. Be on the lookout for more information in the Fall!
Read Full May 2024 Edition of Medicine Matters
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, In the Know, News and Notes, Notable Achievements, Publications, Research, Top News
