 Message from Imre Noth MD, Pulmonary & Critical Care Division Chief
Message from Imre Noth MD, Pulmonary & Critical Care Division Chief
This past year has had its “ups” and “downs” for the Division of Pulmonary and Critical Care Medicine. But we continue to move forward stronger than ever, growing on all fronts, most notably with a new Bedside Procedure Service that began in the fall while caring for the sickest and most complex populations in the MICU. Our research efforts continue to be rewarded with new grants and exciting discoveries, and our presence in the outpatient setting has been steady.
But I would be very remiss if I did not mention the toll of the passing of Dr. H. Charles Malpass in September. His loss was sudden and still very much felt among all the faculty. As our bronchoscopy director, he led tremendous growth in interventional pulmonary medicine with Dr. Subodh Pandey. I’d also like to shout out to Subodh and Dr. Kat Egressy for keeping things afloat while we seek to recruit new members to our IP group. In this issue, you’ll find an update on the Charles Malpass Memorial Grand Rounds to be held on May 24th of this year. We hope that you’ll be able to attend with our guest speaker and former faculty, Dr. Cynthia Brown.
On other fronts, Dr. Hitesh “Heath” Patel and Dr. Jeff Sturek have stepped up as Director and Associate Director for our exciting new inpatient procedures service. Using the principle of conducting procedures at the bedside, they have taken the “bull by the horns” by conducting central lines, paracenteses, thoracentes, etc., at the bedside. This service is designed to provide a timely response while enhancing resident and medical student teaching for these critical procedures. Several institutions have found this service to accelerate patient care greatly.
In this issue, you’ll find several other exciting updates, including Dr. Sturek’s oncopulmonary clinic and research updates from Dr. Cathy Bonham. Our research accomplishments continue to flourish yearly, with more publications and grant awards! And some have even made the lay press, as with John Kim’s publication on the role of Omega 3 fatty acids in ILD.
All in all, I’m pretty excited to see what the next year brings!
~ Imre Noth MD
Clinical Update
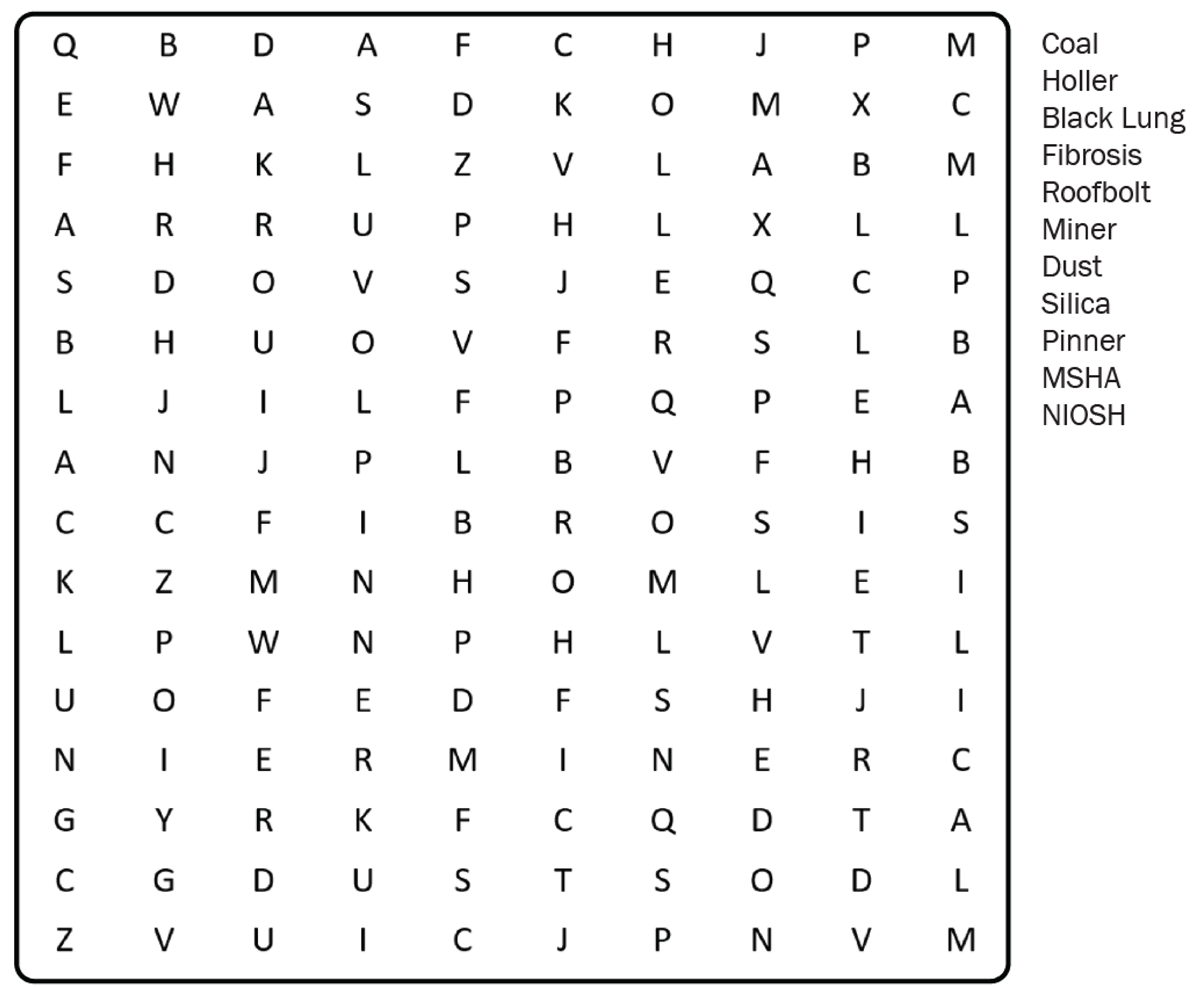
Update from the Coalfields of SWVA
Coal mining continues its decline in the US in favor of cheaper and greener forms of energy production. However, black lung disease rates have surged in the last two decades – concentrated in SW Virginia. Drew Harris, UVA Pulmonologist, is working to reverse these disease trends and care for patients with black lung. Drew serves as medical director of the Stone Mountain black lung program, the only federally funded black lung clinic in Virginia and the largest black lung clinic in the country. The Stone Mountain program includes a pulmonary clinic, a pulmonary rehabilitation center, a pulmonary function testing laboratory, and a black lung benefits program.
The Stone Mountain Black Lung team has been engaged in federal advocacy efforts to improve workplace protections and prevent future diseases. In addition, the Black Lung team at Stone Mountain has recently elucidated a mental health crisis in current and former coal miners. It is partnering with many other clinics and departments around the country (including UVA psychiatry) to help improve mental health outcomes in miners. Drew recently became a CDC/NIOSH certified “B-reader,” meaning he will now interpret chest X-rays to determine the presence and progression of pneumoconiosis in miners.
Over the last six years, Drew’s hair has turned grey while he logged over 60,000 miles (320 miles in each direction) driving to/from the Stone Mountain black lung clinics in Lee and Buchanan County. Although he does utilize telemedicine to supplement these in-person trips, he welcomes anyone in the DOM with a pilot license and access to a plane to shorten his commute / lengthen his telomeres.
New Inpatient PCCM Bedside Procedures Service
We were thrilled to have launched the Pulmonary and Critical Care Medicine Bedside Procedures Teaching Service this past October 24th, 2023, with support from the internal medicine residency and collaboration with interventional radiology and neuroradiology divisions. The purpose of the service is to help improve inpatient patient care, resident procedural education, and operational efficiency at our medical center.
Prior studies have demonstrated that Medicine Bedside Procedure Services (MPS) benefit patients, resident physicians, attending physicians, and hospital operational efficiency (see Figure 1).
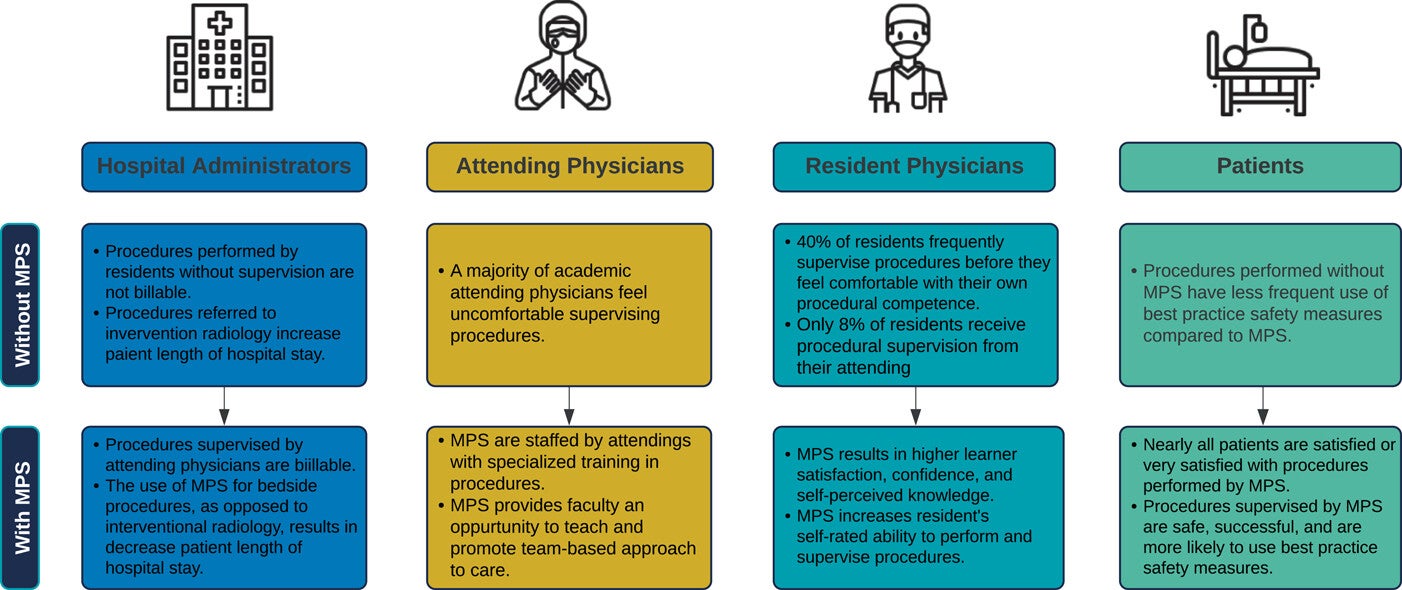
Figure 1 from Buell KG, Hayat MH, Walsh DW, Wooldridge KT, Vasilevskis EE, Heller LT. Creation of a medical procedure service in a tertiary medical center: Blueprint and procedural outcomes. J Hosp Med. 2022; 17: 594-600. doi:10.1002/jhm.12901
Our service is available on weekdays from 8 am to 5 pm (excluding holidays). It offers a variety of procedures at the bedside, including lumbar punctures, paracenteses, thoracentesis, pigtail chest tube placement, and central venous catheter placement. A resident performs the procedures under attending supervision across the medical center (including floor, step-down, and intensive care units). We pride ourselves on rapidly performing procedures to ensure rapid diagnosis and alleviation of patient symptoms. Procedures are typically completed within 2 to 3 hours of consultation.
We are eager to continue growing the service and make it a resounding success. We look forward to your support in enhancing our patients’ experiences, resident education, and improving the operational efficiency of our medical center. Please get in touch with Heath Patel (hhp3n@uvahealth.org) or Jeff Sturek (jms3hk@uvahealth.org), the service line medical directors, with any questions.
Update from Oncopulmonary
Dr. Sturek has continued to develop the Oncopulmonary Clinic, focusing on caring for patients with a wide array of pulmonary complications from the treatment of malignancy, including chemotherapy, immune checkpoint inhibitors, radiation therapy, and hematopoietic stem cell transplant. He is the pulmonary specialist on the recently formed Immune-Related Toxicity (irTOX) Team, an eConsult-based service led out of the Division of Hematology and Oncology by Drs. Sean Dougherty and Richard Hall, advising on suspected immune checkpoint inhibitor-related pneumonitis cases. Additionally, he collaborates with the Hematopoietic Stem Cell transplant team, led by Dr. Wagner, in pre-transplant pulmonary evaluation and management of post-transplant complications. Dr. Sturek has focused research interests on pulmonary complications following stem cell transplant and is a member of an international consortium on Lung Graft-versus-Host Disease (GVHD) led by Dr. Guang-Shing Cheng at Fred Hutchinson Cancer Center in Seattle. His lab is working to understand the immunologic mechanisms of serositis-type GVHD, a project led by DOM trainees Drs. Frank Papik (PCCM Fellow) and Rebecca Brown (Medicine Resident).
Research Update
Interstitial Lung Disease (ILD) remains a focus for several faculty members. Dr. John Kim had a particularly spectacular 2023, with multiple first-author publications reporting on the association of plasma omega-3 fatty acids with progression and survival from idiopathic pulmonary fibrosis (IPF) and factors that impact the evolution of interstitial lung abnormalities. Dr. Kim has found early radiographic interstitial lung abnormalities associated with poorly controlled sleep apnea, hiatal hernias, and genetic susceptibility risk factors such as the MUC5B promoter variant and chromosome telomere length: division chief Dr. Imre Noth, Drs. Kim, Shwu-Fan Ma, and Yong Huang published data from the multicenter CLEANUP-IPF trial demonstrating that increasing buccal microbial diversity predicts worse IPF severity and survival. In other publications, the group identified a proteomic biomarker and four novel gene variants for IPF survival, including one in PCSK6 that reached genome-wide significance. A novel cluster analysis of transcriptomic datasets yielded endotypes of IPF, supporting our observations of clinical heterogeneity even within the group of patients diagnosed with IPF. The UVA ILD group, including Drs. Huang, Ma, Kim, Noth, Cathy Bonham, Andrew Barros, and Anne Sperling, also published on the heterogeneity of the IPF lung, demonstrating marked differences in gene expression and myofibroblast features in central versus peripheral lung tissue.
Dr. Anne Sperling’s lab is actively studying the role of lung-draining mediastinal and hilar lymph nodes in disease pathology of asthma, pulmonary fibrosis, and lung injury. The lab reported that dendritic cells prime naive CD8(+) T cells in situ before migration to draining lymph nodes and that dendritic cells play a role in acute graft versus host disease. Dr. Sperling and collaborators have also identified key cytokine signatures for patients with septic shock. The American Thoracic Society recently invited Dr. Sperling to serve on an international workshop panel, Building Career Paths for Ph.D., Basic and Translational Scientists in Clinical Departments in the United States.
Dr. Jeff Sturek’s lab studies B cell responses in pulmonary fibrosis and lung injury. In the Sturek lab, Dr. Riley Hannan, PhD, was awarded a Ruth L. Kirschstein F32 Postdoctoral Individual National Research Service Award from the NHLBI for his project entitled “Role of Natural Antibodies and B1 cells in Fibroproliferative Lung Disease”. Dr. Eva Otoupalova, MD, was appointed as a postdoctoral fellow to the IGNITE KUH Training Program, which has supported her collaborative work with Dr. Scott Heysell from the Division of Infectious Diseases on the role of B cells and emergency myelopoiesis in HIV-related TB sepsis in Tanzania and Uganda.
Our Cystic Fibrosis Center of Excellence, directed by Dr. Dana Albon, led the field in the adoption of telemedicine and recently published its experience. Dr. Albon has also collaborated closely with our colleagues in the Division of Allergy and Immunology, resulting in a fascinating publication on the impact of CFTR modulator triple therapy on type 2 inflammatory response in patients with cystic fibrosis.
Drs. Max Weder, Hannah Mannem, and Charlie Alex met the challenge of COVID-19 by managing some of the first lung transplants for COVID-19 in the United States. The UVA Lung Transplant team experience was published by Dr. Weder in 2023, Lung Transplantation for COVID-19-related Lung Disease: Clinical Experience and Call for a Global Registry. 1-year results of the international COVID lung transplant database, including over 100 patients, are under review, demonstrating that survival is comparable to other lung transplant indications. Still, infectious complications are common in the early post-transplant period.
Dr. Eric Davis has co-authored an International Consensus Statement on Obstructive Sleep Apnea in sleep medicine. Dr. Davis also reported on the association of disrupted sleep with 24-hour blood pressure variability in caregivers and collaborated with others to test a mouse model for Intensive Care Unit delirium, producing data on sleep fragmentation, electroencephalographic slowing, and circadian disarray.
Publications by the pulmonary critical care faculty show the importance of early interventions and longitudinal follow-up for COVID-19. Drs. Taison Bell, Enfield, Barros, and current fellows Drs. Christian Widere and Claire Davis published early empiric antibiotic use in COVID-19. Dr. Sturek published the clinical trial results of the Angiotensin-II vasopressor in JAMA. In the lab, Dr. Sturek and Dr. Lindsay Somerville collaborated to report on inhibiting the mitochondrial pyruvate carrier, mitigating hyperinflammation and hyperglycemia in COVID-19. In longitudinal follow-up studies, Drs. Alex Kadl, Eric Davis, Kyle Enfield, current fellow Dr. John Popovich, and recent fellowship graduates Drs. Sam Oliver and Sam Lazoff reported on chronic neurocognitive and pulmonary symptoms in COVID-19. For our sickest patients, Drs. Kadl, Enfield, and graduate Dr. Chintan Ramani published on early posthospitalization recovery after extracorporeal membrane oxygenation for COVID-19. Current fellows Dr. Claire Davis and Dr. Enfield published their novel “ICU Bundle Board,” a quality improvement initiative that improves care for all MICU patients.
Educational Updates
It has been another successful year for the fellowship program!

Graduation 2023 at Morven Farm, front row from left: Dr. Cathy Bonham (Associate Program Director), Drs. Eva Otoupalova, and Daisy Zhu; Back row from left: Drs. Sam Oliver, Sam Lazoff, and Dr. Tim Scialla (Program Director). Movie night seeing Lost Boys – the irony was not lost on participants.

From left: Drs. Tim Scialla (PD), Christian Widere, Frank Papik, and Eric Polley. During orientation, our fellows attended a Bronchoscopy course at Duke University.

Recently, our first-year fellows participated in Research Week, where they met many wonderful faculty mentors. From left: Drs. Sam Konkol, Matt Freedman, Frank Duerson, and Christian Widere.

On the last day of orientation, we take our fellows for a hike at Humpback Rock. The view from the top is worth the uphill trek!
From left: Drs. Frank Duerson, Christian Widere, Matt Freedman, and Sam Konkol.

From left: Drs. Christian Widere, Matt Freeman, Frank Duerson, Sam Konkol, and Cathy Bonham (APD).
Events
UPCOMING: H. Charles Malpass III Memorial Grand Rounds
Together with the Department of Medicine, the Division of Pulmonary and Critical Care will host the inaugural H. Charles Malpass III Memorial Grand Rounds on Friday, May 24, 2024, in honor of the late Dr. Howard Charles Malpass III (Charlie). Dr. Malpass, an amazing father, husband, brother, son, runner, and clinician, passed away suddenly on September 14, 2023.
Charlie was renowned for his dedication as a pulmonary physician at UVA Health, specializing in interventional pulmonary and bronchoscopy. He tirelessly worked to provide diagnostic lung results and guidance for patients’ treatment, even while facing his own battle with acute myeloid leukemia (AML). On the very day of his AML diagnosis, he selflessly called patients with reassuring news. His colleagues highly esteemed him for his humor, brilliance, and compassionate care.
The inaugural Grand Rounds will feature Dr. Cynthia Brown from Indiana University in honor of Charlie’s legacy. Dr. Brown was on faculty at UVA during Charlie’s fellowship and, like Charlie, is held in esteem for her dedication to fellow education and patient care. Stay tuned for more details on the events surrounding the Grand Rounds as we remember Dr. Malpass and celebrate his enduring impact on the medical community.
ATS Alumni & Friends Reception
In May 2023, the division hosted a networking social at the ATS International Conference in Washington, D.C. Faculty, fellows, alums, colleagues, and friends gathered at City Tap to enjoy light fare and catch each other up on job opportunities, upcoming research, and other interests.
 Holiday Party
Holiday Party
In December 2023, PCCM had its annual Holiday Party. To mix things up and try a fun new place, we went to Firefly Barcade, which had food, music, games, and karaoke. We had a fantastic turnout from faculty, fellows, and staff. We rang in the holiday season and saw the fun from the division.
ILD Patient Education Day 2023
Interstitial lung disease (ILD) is a heterogeneous group of diseases that range from rheumatoid lung disease to sarcoidosis to devastating idiopathic pulmonary fibrosis (IPF), which has a median survival of 2-5 years. The UVA ILD program offers comprehensive, longitudinal, and multidisciplinary care for this complex population.
One of the key aspects of the care of patients with ILD is patient education. In addition to a biweekly patient support group under the leadership of Drs. Tessy Paul and Catherine Bonham, the team held its fifth annual ILD Patient Education Day on September 9, 2023. The theme was “Through the Looking Glass” and featured keynote speaker Dr. Sydney Montesi, a nationally renowned ILD expert from Harvard Medical School.
Additional topics discussed included new imaging techniques for Pulmonary Fibrosis, autoimmune and sarcoid-associated lung disease, and clinical trials in ILD. This hybrid event was accessible virtually and in person with support from the PFF and had overwhelmingly positive responses from patients and their caregivers.
SELECT PUBLICATIONS
Huang, Y., Guzy, R., Ma, S. F., Bonham, C. A., Kim, J. S., Barros, A. J., Sperling, A. I., Noth, I. et al. (2023). “Central lung gene expression associates with myofibroblast features in idiopathic pulmonary fibrosis.” BMJ Open Respir Res, 10(1).
Jamil, R., Goins, T., Partlow, K., Barger, K., & Mihalek, A. D. (2023). “Application of the Plan-Do-Study-Act method to optimize the ordering and administration of dexmedetomidine for sleep hygiene in the intensive care unit.” Am J Health Syst Pharm, 80(Suppl 3), S97-S102.
Kalinina, O., Minter, L. M., Sperling, A. I., Hollinger, M. K., Le, P., Knight, K. L. et al. (2024). “Exopolysaccharide-Treated Dendritic Cells Effectively Ameliorate Acute Graft-versus-Host Disease. Transplant Cell Ther,” 30(1), 79 e71-79 e10.
Kim, J. S., Azarbarzin, A., Podolanczuk, A. J., Anderson, M. R., Redline, S. et al. (2023). “Obstructive Sleep Apnea and Longitudinal Changes in Interstitial Lung Imaging and Lung Function: The MESA Study.” Ann Am Thorac Soc, 20(5), 728-737.
Kim, J. S., Kim, J., Yin, X., Hiura, G. T., Noth, I., Manichaikul, A., Oelsner, E. C. et al. (2023). “Associations of hiatus hernia with CT-based interstitial lung changes: the MESA Lung Study.” Eur Respir J, 61(1).
Kim, J. S., Ma, S. F., Ma, J. Z., Huang, Y., Bonham, C. A., Noth, I. et al. (2023). “Associations of Plasma Omega-3 Fatty Acids With Progression and Survival in Pulmonary Fibrosis.” Chest.
Kim, J. S., Manichaikul, A. W., Noth, I., Garcia, C. K., Podolanczuk, A. J. et al. (2023). “MUC5B, telomere length and longitudinal quantitative interstitial lung changes: the MESA Lung Study” Thorax, 78(6), 566-573.
Kraven, L. M., Taylor, A. R., Huang, Y., Noth, I., Ma, S. F., Yeo, A. J., Fahy, W. A., Jenkins, R. G., & Wain, L. V. et al. (2023). “Cluster analysis of transcriptomic datasets to identify endotypes of idiopathic pulmonary fibrosis. Thorax,” 78(6), 551-558.
Mehta, A. M., Lee, I., Li, G., Jones, M. K., Hanson, L., Lonabaugh, K., List, R., Borish, L., & Albon, D. P. (2023). “The impact of CFTR modulator triple therapy on type 2 inflammatory response in patients with cystic fibrosis” Allergy Asthma Clin Immunol, 19(1), 66.
Moore, B. B., Ballinger, M. N., Prakash, Y. S., Sperling A.I., Konigshoff, M. et al .(2023). “Building Career Paths for Ph.D., Basic and Translational Scientists in Clinical Departments in the United States: An Official American Thoracic Society Workshop Report.” Ann Am Thorac Soc, 20(8), 1077-1087.
O’Dwyer, D. N., Kim, J. S., Ma, S. F., Huang, Y., Gilbert, J. A., Martinez, F. J., & Noth, I. et al. (2023). “Commensal Oral Microbiota, Disease Severity and Mortality in Fibrotic Lung Disease.” Am J Respir Crit Care Med.
Oldham, J. M., Allen, R. J., Kim, J. S., Huang, Y., Noth, I. et al. (2023). “PCSK6 and Survival in Idiopathic Pulmonary Fibrosis.” Am J Respir Crit Care Med, 207(11), 1515-1524.
Oldham, J. M., Huang, Y., Ma, S. F., Kim, Noth, I. et al. (2023). “Proteomic Biomarkers of Survival in Idiopathic Pulmonary Fibrosis.” Am J Respir Crit Care Med.
Oliver, S. F., Lazoff, S. A., Popovich, J., Enfield, K. B., Quigg, M., Davis, E. M., & Kadl, A. (2023). “Chronic Neurocognitive, Neuropsychological, and Pulmonary Symptoms in Outpatient and Inpatient Cohorts After COVID-19 Infection.” Neurosci Insights, 18, 26331055231186998.
Self, W. H., Shotwell, Sturek, J. M., Levitt, J., et al. (2023). “Renin-Angiotensin System Modulation With Synthetic Angiotensin (1-7) and Angiotensin II Type 1 Receptor-Biased Ligand in Adults With COVID-19: Two Randomized Clinical Trials.” JAMA, 329(14), 1170-1182.
Sharp, M., Mustafa, A. M., Farah, N., & Bonham, C. A. (2023). “Interstitial Lung Disease and Sarcoidosis Health Disparities.” Clin Chest Med, 44(3), 575-584.
Si, Y., Wang, Y., Tian, Q., Wang, Q., Sperling, A. I., Chong, A. S. et al. (2023). “Lung cDC1 and cDC2 dendritic cells priming naive CD8(+) T cells in situ prior to migration to draining lymph nodes.” Cell Rep, 42(10), 113299.
Taylor, L. J., Jolley, S. E., Ramani, C., Kadl, A., Enfield, K., Zwischenberger, J. B., Rove, J. Y. et al. (2023). “Early posthospitalization recovery after extracorporeal membrane oxygenation in survivors of COVID-19.” J Thorac Cardiovasc Surg, 166(3), 842-851 e841.
Weder, M. M., Aslam, S., & Ison, M. G. (2023). “Lung Transplantation for COVID-19-related Lung Disease: Clinical Experience and Call for a Global Registry. Transplantation,” 107(1), 18-20.
Widere, J. C., Davis, C. L., Loomba, J. J., Bell, T. D., Enfield, K. B., Barros, A. J., et al. (2023). “Early Empiric Antibiotic Use in Patients Hospitalized With COVID-19: A Retrospective Cohort Study.” Crit Care Med, 51(9), 1168-1176.
Zhao, J. O., Patel, B. K., Krishack, P., Kress, J. P., Hall, J. B., Sperling, A. I., Adegunsoye, A., Verhoef, P. A., & Wolfe, K. S. et al. (2023). “Identification of Clinically Significant Cytokine Signature Clusters in Patients With Septic Shock.” Crit Care Med, 51(12), e253-e263. https://doi.org/10.1097/CCM.0000000000006032
Zhu, B., Wei, X., Narasimhan, H., Braciale, T. J., Somerville, L., Colca, J. R., Pandey, A., Jackson, P. E. H., Mann, B. J., Krawczyk, C. M., Sturek, J. M., & Sun, J. et al. (2023). “Inhibition of the mitochondrial pyruvate carrier simultaneously mitigates hyperinflammation and hyperglycemia in COVID-19.” Sci Immunol, 8(82), eadf0348.
Davis CL, Bjoring M, Hursh J, Smith S, Blevins C, Blackstone K, Nicholson E, Hoke T, Michel J, Noth I, Barros A, Enfield K. The Intensive Care Unit Bundle Board: A Novel Real-Time Data Visualization Tool to Improve Maintenance Care for Invasive Catheters. Appl Clin Inform. 2023 Oct;14(5):892-902. doi: 10.1055/a-2165-5861. Epub 2023 Sep 4. PMID: 37666277; PMCID: PMC10651369.
Dulko E, Jedrusiak M, Osuru HP, Atluri N, Illendula M, Davis EM, Beenhakker MP, Lunardi N. Sleep Fragmentation, Electroencephalographic Slowing, and Circadian Disarray in a Mouse Model for Intensive Care Unit Delirium. Anesth Analg. 2023 Jul 1;137(1):209-220. doi: 10.1213/ANE.0000000000006524. Epub 2023 May 16. PMID: 37192134
Read entire March 2024 Edition of Medicine Matters
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, Expressions, In the Know, New Faces, New Places, News and Notes, Notable Achievements, Publications, Research, Top News
