Message from Mohan Nadkarni MD, Division Chief, General, Geriatric, Palliative & Hospital Medicine

I am pleased to highlight some exciting events our division provides to our patients and community. We have a broad array of faculty, APPs, and staff with interests that span everything from care of our elderly patients, terminally ill patients, primary care patients, unhoused patients, patients at home, outpatients, inpatients, and everywhere in between. We highlight advances in providing colon cancer screening, community outreach, and excellence in clinical care. Many of our clinicians were recently recognized with patient satisfaction awards – it is easy to see the clinical dedication our section provides.
Educationally, our Palliative and Geriatric fellowships are thriving. We also highlight the work of Drs. Lehtinen and Kon with the Patient Student Partnership Program, in which all 160 first-year medical students are paired with actual patients they follow throughout their medical school training. It is a joy to lead and work with such a dedicated, innovative, and friendly group of people who provide such excellent care and education to so many.
~ Mohan Nadkarni, MD, Division Chief
Program Updates
Enhancing Connections for Patients Experiencing Homelessness Post-Discharge

By Matthew Allen MD
Education Updates
Patient Student Partnership Program
 By Simon Lehtinen MD
By Simon Lehtinen MD
Entering its sixth year, the Patient Student Partnership (PSP) is a longitudinal patient experience for the University of Virginia School of Medicine students. In the program, all incoming first-year medical students are paired with a patient experiencing chronic illness. Students follow their patients throughout their medical school careers, attending clinic appointments and procedures, visiting their patients in the hospital, and checking in regularly.
Including “partnership” in the program’s name is not accidental, as the course benefits students and their patients. Students gain clinical experience early in their medical school careers. By witnessing the longitudinal care of a patient over three and a half years, students observe firsthand both the trajectory of chronic illness and the social determinants of health that affect medical care. The program gives context to what students learn in their basic science courses by applying these concepts to patient care. Additionally, students develop communication skills and experience their first professional relationship with a patient, a foundation for patient-doctor relationships in the future.
PSP allows students to become authentic members of the healthcare team. Students advocate for patients by connecting them with resources, helping them navigate the complex healthcare system, and helping patients organize their medical care. In addition to receiving these benefits, many of our patients welcome the opportunity to teach and help shape the next generation of physicians.
The patients come from various clinics across the UVA health system, including many Department of Medicine clinics—UMA, UPC, Heart and Vascular, the Ryan White HIV Clinic, Pulmonary, GI, and Renal, to name a few. When possible, we pair students based on their areas of interest, whether it be a particular medical specialty or working with a specific population.
On July 1st of this year, I took over as course director. To say that I took over a well-run and well-thought-out program is an understatement, with many thanks to the Department of Medicine faculty. Dr. Peggy Plews-Ogan developed the Phronesis program from which PSP developed. Dr. Rachel Kon took over the program’s leadership subsequently, overseeing the program’s expansion to all four classes of students in the School of Medicine. In my new role, I am building on this foundation, introducing a new curriculum, and expanding the clinics and programs from which patients are recruited.
It’s certainly worth mentioning that without the program’s patient volunteers, clinics, and clinician support, our medical students could not have this experience. Thank you to everyone who has contributed to this program by volunteering to help patients, teaching small group sessions, and welcoming medical students into the clinical space. If you know patients interested in participating in the program or would like to learn more, please get in touch with Simon Lehtinen at sl4ee@uvahealth.org, or our program coordinator, Rachel Smith, at patientstudentpartnership@virginia.edu.
Virginia Hospice and Palliative Fellowship Program Update
 By W. Nat Timmins MD
By W. Nat Timmins MD
The University of Virginia Hospice and Palliative Fellowship Program was delighted to welcome our AY 2023-2024 fellows in July 2023: Maki Nakazato, MD, and Kellie Mitchell, MD. Dr. Nakazato comes to us from California. She completed her undergraduate degree at UCLA and then moved east to get her medical degree from Thomas Jefferson University. She stayed in Philadelphia for her residency in Family Medicine. Afterward, she returned to the West Coast for a fellowship in Geriatrics at Stanford, which she completed in June 2023. Maki loves to sing and read Japanese novels. You might recognize Dr. Mitchell because she finished her UVA Emergency Medicine Residency in June 2023. She has a BS in Biochemistry from Mississippi State University and completed her medical degree from the University of Alabama at Birmingham. When not practicing medicine, Dr. Mitchell is creating and active. She has competed in aerial dance and enjoys music, painting, and writing poetry and fiction.
We are busy interviewing for an AY 2024-2025 fellow. We are honored to have many strong applicants for the fellowship again. Though we will only have one fellow in AY 2024-2025, we have had 39 applications thus far.
Our one-year fellowship packs a lot of clinical experiences for our fellows in the inpatient palliative consultation setting, the outpatient Palliative Care Clinic setting in the Emily Couric Clinical Cancer Center, and in hospice care with our great partner – Hospice of the Piedmont. In addition, our fellows rotate with radiation oncology, interventional pain, and pediatric palliative care colleagues at UVA. We seek to leverage diversity in our fellows to create well-rounded Hospice and Palliative Medicine clinicians who are prepared for academic practice, community practice, or both. We additionally hope to train clinicians who could thrive in the Commonwealth of Virginia. Many of our fellowship graduates continue improving end-of-life care in Charlottesville; several hospice physicians, including the current Chief Medical Officer at Hospice of the Piedmont, trained with us at UVA.
Clinical Updates
UMA’s Colorectal Cancer Screening Initiative: Progress and Future Plans
 By David Callender MD
By David Callender MD
UMA is committed to increasing colorectal cancer screening rates in partnership with the Community Outreach and Engagement team at the Cancer Center and University of Virginia Digestive Health. With support from an American Cancer Society Grant in 2022, the clinic implemented a quality improvement project to increase the number of FIT stool-based tests returned to the clinic. Before the intervention, the clinic’s FIT return rate was 41%. To help address this, a two-step RN-led navigation process was introduced. Patients who did not return their FIT tests within two weeks of their clinic visit were automatically directed to a nurse navigator. This navigator made a phone call attempt to contact the patient and assist in overcoming any barriers preventing the test’s return. If the initial call went unanswered, a voicemail was left, and a letter was dispatched to remind the patient to return their FIT test. By the end of the pilot, the return rates for FIT tests increased to 66%. The success led UMA to sustain this navigation service.
Based on the success of this first grant in 2022, the ACS gave additional funding, “ACS 2023 Quality Improvement Screening Project,” with Wendy Cohn as PI, Dr. Cindy Yoshida, and Dr. David Callender as Co-PIs. The efforts have taken two significant directions in 2023:
Hispanic Patient Navigation – We have broadened the two-step navigation to serve our Hispanic population. The Hispanic navigation adapts the original nurse-led protocol to be delivered in Spanish by a non-clinical navigator, addressing the everyday barriers faced by the Hispanic population when completing screenings. Although the Hispanic navigation protocol has been in place for only four months, initial data is promising. Three months into the program, 46.2% of those who hadn’t returned a FIT within the two-week window after their clinic visit did so after undergoing the navigation protocol.
QI Project to Address CRC Screening Disparities at UMA – We have initiated a new QI initiative targeting under-screened patients aged 45-49. The grant’s second intervention aims to reach the under-screened 45-49 age group through a mailed FIT test campaign disseminated via MyChart (and traditional mail for those not on MyChart). Patients lagging in their colorectal cancer screening will receive a message emphasizing the importance of the screening and a notification about a forthcoming FIT test in the mail. They will also have the choice to opt out of this mailing through MyChart. Those who don’t return the mailed FIT will be integrated into our standard navigation protocol. This initiative is slated to commence this fall.
UMA is dedicated to continuous improvements in community health, and with these initiatives, we hope to create lasting impacts beyond our clinic. We sincerely acknowledge our Gastroenterology Division partners in this work, including Lindsay Hauser, Wendy Cohn, and Cindy Yoshida.
Awards and Recognition
We proudly recognize and celebrate many of our dedicated colleagues and their accomplishments!
American College of Physicians Masterships
Every year, the American College of Physicians, the national society of 161,000 Internal Medicine physicians, awards 50 Masterships. There are 13 living Masters in Virginia, including Drs. Reynolds, Rosner, and Wolf. This year, the ACP recognized three of our faculty. Dr. Stewart Babbott (GIM) and Dr. Mohan Nadkarni (GIM & former IM/UMA resident) were awarded a Mastership in AC P. Each year, there is one national awardee for the Waxman Award for Outstanding Contribution to Medical Education. That honor goes to Dr. Andrew Parsons (Hospital Medicine and former IM/UMA resident) this year! It is quite historic for any institution to have three members selected for these national awards in one year! Please join us in congratulating these faculty members on this notable achievement!
Charles L. Brown Award for Patient Care Quality
“The Charles L. Brown Award for Patient Care Quality was established in 2006 to honor Mr. Brown’s service and generosity to UVA Health as a former member of the Health System Board. Through this fund, $10,000 is awarded annually to a Medical Center team to recognize excellence in patient care improvement in the areas of Quality and/or Patient Safety. The funds shall be used by the winning team for continuing professional education with a focus on efforts to provide superlative care and service to our patients.”
This year’s Charles L. Brown Award recipient was University Physicians Orange. Their project entitled “Success in Transitional Care Management” earned this recognition from UVA Health based on their results in reducing hospital readmission rates.
DOM Clinical Excellence Award
Karen Duffy
Terri Artale
Beth Jaeger-Landis
Dean’s Award for Clinical Excellence – Ira Helenius
Academic Medicine Reviewer Award for the Academic Medicine Journal – Stewart Babbott
Special shout out to our APP’s that are up for awards!
Exceptional APP Award Nominees
Beth Jaeger-Landis
Karen Duffy
Excellence in Scholarship Award Nominee – Caitlin Burchfield
Patient Experience Awards
GENERAL MEDICINE:
Deborah Adams
Teresa Artale
Stewart Babbott
Maria Badaracco
Ken Ballew
David Callender
Brittany Cavanaugh
Lien Dame
Kim Dowdell
Jeannine Engel
Tabor Flickinger
Matt Goodman
Evan Heald
Katie Jaffe
Rachel Kon
Simon Lehtinen
John MacKnight
Andy Wolf
GERIATRICS:
Rebecca Mullan
Karen Starr
Christina Tieu
Promotions
Tabor Flickinger – Associate Professor
Katie Jaffe – Associate Professor
Justin Mutter – Associate Professor
Positions Achieved
Mohan Nadkarni – Leadership Council of the Society for General Internal Medicine / GIM National Association
David Callender – Representative to the Virginia ACP Governors Council
Grants
Laurie Archbald-Pannone
2022-2024 – Virginia Long-Term Care Infrastructure Pilot Projects (VLIPP) – HAIAR, CDC Nursing Home Strike force funding: Virginia Infection Control Center of Excellence (VICE), Total estimated funding $1,210,312 over 2 years ($ 605,156 with 1 one-year renewal period, (Grant support: PI: 20% FTE/ year)
2021-2023 – West Health Institute Collaborative Funding, “UVA-WHI Geriatric Telemedicine Resource Development $265, 000 award over two years (Grant support: PI 12-15% FTE/year)
2020-2025 – ACT Trial: Alanyl-glutamine Supplementation for Clostridioides difficile in Elderly, Phase 2 Clinical Research Trial (Grant support: 10% FTE/year).
Grant Projects in Process
2023-2024 – Coulter Translational Partnership, “Model-driven design of microbial therapies to resolve C. difficile infection.” PI: Jason Papin (BME), L Archbald-Pannone (DOM), Co-I Glynis Kolling (BME). $153,000, REVIEW PENDING (Grant support: 3% FTE/year).
Leslie Blackhall
Betty Irene Moore Fellowship for Nurse Leaders and Innovators:
Developing and Testing a Novel Mobile Health Solution (CommSense) to Improve Patient-Provider Communication
Role: Co-I (Virginia LeBaron, PI)
Amount: $450,000
Dates: 7/1/23 – 6/30/26
NINR RO1: Characterizing the complexity of cancer pain in the home context by leveraging smart health technology. Role: Co-I. 2/1/21-11/30/25. $3,419,796
PCORI: REACH PC: Comparative Effectiveness of Early Integrated Telehealth Versus In-Person Palliative Care for Patients with Advanced Lung Cancer Role: Co-Investigator and Site Lead for multi-site national study 1/2018 – 1/2023
$10,957,491.
Milad Memari
Thomas Nimick, Jr. Foundation Grant, Shadyside Foundation, Pittsburgh, PA
For the project entitled ‘Development and Psychometric Validation of a Social Determinants of Health, Competency-Based Objective Structured Clinical Examination.’
Duration 01/01/2022 – 12/31/2023
Thank you to Cyndi Smith-Powers
The Division Administrative Team would like to express its appreciation for Division Administrator Cyndi Smith-Power’s unwavering support, leadership, and sense of humor. She has led the Team with dedication, hard work, and long hours during a period of turnover, vacancies, and extended absences. We are grateful to her for always knowing when to push and when to pause and when the Team needed a release or recognition and encouraging us to strive to be better human beings. Thank you, Cyndi, for being such a dynamic leader!
 Celebrating the Best, Dr’s. Schectman, Voss and Scott
Celebrating the Best, Dr’s. Schectman, Voss and Scott

Celebrating Ourselves
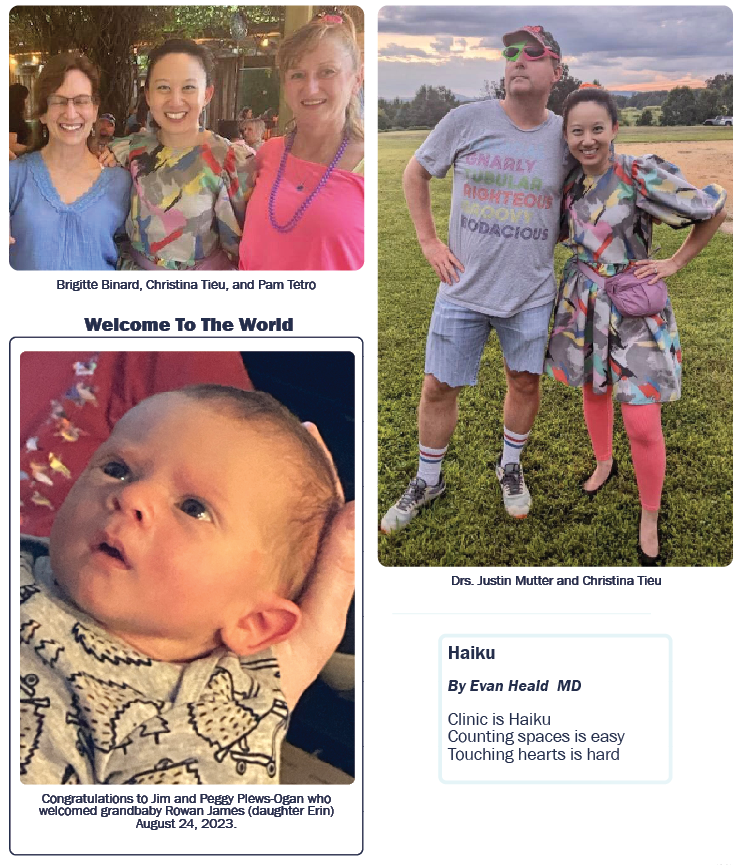
On September 17th, 2023, the Division gathered at Three Notch’d Craft Kitchen to celebrate the start of the new academic year, welcome new colleagues, and visit with those we don’t get to see often. Seeing so many of our Division faculty and staff in attendance with their families was heartwarming. While the food and drink were much appreciated, the balloon artist, Freckles-N-Friends, was the biggest hit with the young and not-so-young kids!



View the entire October 2023 Edition.
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, In the Know, New Faces, New Places, News and Notes, Notable Achievements, Publications, Research, Top News
