Message from Amber Inofuentes, MD, Hospital Medicine Section Head
What a year! 2022 has been another busy and productive one for the section of Hospital Medicine.
Though periodic COVID surges continued throughout the year, adapting clinical operations to meet census and staffing needs became routine. Our surge plans had now weathered two years of volatile inpatient volumes; swells in patient census or physician illness that once created operational panic became a manageable rhythm in hospital medicine, allowing us to expand our focus to other critical strategic aims.
In continuing education and faculty development, we implemented a new mentorship model for all faculty, began a Hospital Medicine Grand Rounds series, and launched the Early Career Scholars program as an opportunity for junior faculty to develop an academic niche. Two more of our faculty members (Andrew Parsons and Shri Gadrey) were also successfully promoted to Associate Professor.
In the clinical arena, our admitter-rounder model was launched last October and remains highly successful; faculty report satisfaction with its positive impact on daily workload, expanded our admitting capacity during daytime hours, and improved geographic placement of patients with physician teams. This September, we also implemented a significant redesign of our 24-hour operations with the beginning of a second-night hospitalist service.
Our group also remains active in a variety of quality improvement initiatives. This year we utilized our incentive structure to develop focused projects in LOS reduction and high-value care and provide evidence-based modifications to standard order sets. We also promoted individual accountability through the hospitalist performance dashboard and individual quarterly reviews of 7-day hospital readmissions.
I am proud of all that we have accomplished this year, none of which would be possible without the considerable efforts of the section’s leadership team. I encourage you to read articles throughout the Newsletter highlighting their work and to visit our newly revamped Hospital Medicine website (Hospital Medicine – Division of General, Geriatric, Palliative & Hospital Medicine – virginia.edu) to see the full list of faculty and section leadership. A special thank you to Tammy Schlag for leading our website redesign!
This year, we returned to in-person recruitment and have an impressive class of new faculty to boast about. Many of these outstanding physicians are recruits from our residency program, and we were lucky to recruit others from around the country who bring experience in diverse clinical settings. I hope you enjoy reading the faculty profiles of these new colleagues. We have also grown in other ways. The portfolio of research and quality improvement accomplishments, educational leadership roles, and Department/Medical Center roles continues to expand.
Looking into 2023, we are partnering with the residency program and the division of Pulmonary & Critical Care to develop a Medical Procedure Service, launching a faculty development series for new hires, and continuing our quality improvement efforts with a focus on clinical documentation improvement, patient progression, and high-value care.
As a group, we’d like to extend our gratitude to the rest of the Department for its continued support of our endeavors.
~Amber Inofuentes, MD
Hospital Medicine Honors and Awards
Paul Helgerson, MD
2022 – Dean’s Award for Excellence in Clinical Care
Rahul Mehta, MD
2021 – Department of Medicine Award for Excellence in Teaching
Glenn Moulder, MD
2022 – School of Medicine Award for Excellence in Performance Assessment
Alex Millard, MD
2021 – Department of Medicine Award for Excellence in Teaching
Rahul Mehta, MBBS
2021 – School of Medicine Award for Excellence in Performance Assessment
Greg Young, MD
2021 – School of Medicine Award for Humanism in Medicine
Jessica Dreicer, MD
2022 – Department of Medicine Award for Excellence in Clinical Care
Andrew Parsons, MD
2022 – Virginia ACP Chapter Early Career Physicians Award
Glenn Moulder, MD
2022 – Department of Medicine Award for Excellence in Teaching
SNF Discharge Medication Reconciliation Project (Jessica Dreicer, MD and Amber Inofuentes, MD)
2021 – Charles L. Brown Award for Excellence in Patient Care Quality
Gregory Young, MD
2022 – Department of Medicine Award for Excellence in Teaching
Miriam Gomez-Sanchez, MD Establish wellness space for exercise within the hospital for team members
2022 – UVA Health Spark Innovation Competition Winner
George Hoke, MD
2021 – Department of Medicine Award for Excellence in Teaching
CLINICAL HIGHLIGHTS
 By Sara Brumfield MD, Medical Director
By Sara Brumfield MD, Medical Director
3 North Acute
The 3 North Acute unit has risen from what was formally known as the Transitional Care Hospital (TCH). The Transitional Care Hospital was a UVA-operated Long Term Acute Care Hospital (LTACH) serving the needs of patients from all over the state of Virginia and surrounding regions. TCH specializes in ventilator weaning, management of complex respiratory and medical conditions, complex wounds, and other complicated care requiring acute care hospitalization for up to 30 days. In August 2022, our dedicated team of nurses, PCAs, PT/OT, RT, SLP, and physicians moved to the Main UVA Hospital to become 3 North Acute. This move supported enhanced access to consultant services, imaging, and critical care to better support the needs of our patients. 3 North has a similar mission to care for the needs of Virginians with complex medical needs who require longer hospitalizations until they can reach a lower level of care either to Acute Inpatient Rehab, Skilled Nursing, or Home with Home Health. We are currently running an eight-bed unit taking patients from the Medical ICU and other acute care units with hopes to grow the unit later in the year.
 By Amber Inofuentes MD, Section Head
By Amber Inofuentes MD, Section Head
Night 2 Hospitalist Launches
General medicine inpatient volumes rose significantly in 2020 with surges from the COVID-19 pandemic and have remained consistently higher than pre-pandemic volumes. The hospital medicine program expanded direct care services from three teams to as many as eight during the pandemic’s peak and presently staffs five -six direct care teams. To safely provide care for all hospital medicine patients throughout their hospitalization, including overnight, the program added a second-night hospitalist this past September. In addition to supporting overnight coverage of patients, this role expands the admitting capacity of the hospital medicine service and provides direct supervision for general medicine night float residents. To maintain high job satisfaction and work-life balance for faculty hospitalists, we developed nocturnist and hybrid nocturnist roles for new faculty. We implemented a moonlighter model to staff the new Night 2 hospitalist service. Our inaugural team of nocturnists includes recent UVA graduates Val Lollett, Brian Peterson, and Angel Morvant, who are joined by Joe Kerley, a former chief resident at Kansas University. We believe this model will expand hospitalist clinical care services in future years, promote patient safety, and enhance resident education and supervision for night float rotations.
 By Rahul Mehta MBBS, Director
By Rahul Mehta MBBS, Director
Perioperative and Consultative Medicine
Hospitalists work collaboratively with our orthopedic colleagues to provide high-quality care to the full complement of medically complex joint replacement, spine surgery, and orthopedic trauma patients. Over the last year, the core perioperative faculty, which includes George Hoke, Robert Becker, Miriam Gomez-Sanchez, Ryan Wiggins, and Rebecca Corey, have worked on projects that refined patient criteria for the UVA Outpatient Orthopedic Surgery Center and enabled the successful “Premier Level” certification of the UVA Hip Fracture Program by the International Geriatric Fracture society. The latter is an outcome and process-based accolade reserved for only the highest-performing hip fracture programs in the nation.
EDUCATION HIGHLIGHTS
 By Andrew Parsons MD, Associate Section Head for Education
By Andrew Parsons MD, Associate Section Head for Education
UVA Hospital Medicine Early Career Scholars (ECS) Program
The ECS program was launched in early 2022 with support from the DOM with a primary goal of providing structure and support to foster academic achievement in hospitalist faculty. The two-year ECS Program provides protected nonclinical time for selected faculty to complete a mentored project. Projects can focus on clinical research, medical education, clinical operations, developing a novel clinical program, or quality improvement in alignment with departmental and institutional priorities. Preference was given to hospitalists at the assistant professor level, more than a year beyond completion of residency training, and with 100% clinical effort. Selected hospitalists are required to attend the Society for Hospital Medicine (SHM) Academic Hospitalist Academy. Scholarly output is expected in the form of local/regional presentations during year one or two and national presentations during year two or three. Applications were accepted from February 15th to April 15th, and the ECS Program began in September.
Selected Projects 2022
Alexander Lawson, MD
Category: New Clinical Program
“Development of a Hospital Medicine Point-of-Care Ultrasound Program”
Ian Crane, MD
Category: Medical Education
“An Untaught Fundamental: Simulated Pre-rounding in the Advance Clinical Elective”
By Andrew Parsons MD, Associate Section Head for Education
UVA Hospital Medicine Grand Rounds
Hospital Medicine, a national specialty at UVA, fills an important niche within the internal medicine community. To address hospitalists’ specific faculty development needs, last year, we kicked off “UVA Hospital Medicine Grand Rounds.” This monthly series hosts expert speakers on various topics specific to inpatient medicine and provides Category 1 CME. All are welcome!! Speakers to date have included internal and external experts in Behavioral Medicine, Diabetes care, Heart Failure management, Point of Care Ultrasound, Discharge Transitions, and more. Stay tuned for upcoming speakers this year. Sessions take place monthly on Wednesdays from 12:00-1:00, usually in ERC-B—feel free to join us.
By Andrew Parsons MD, Associate Section Head for Education
Hospital Medicine Career Showcase
As part of a rotation within Hospital Medicine Grand Rounds, we began a series called “Career Showcase.” This series aims for successful hospitalists outside of UVA to share their career journey so that our group may learn about different career trajectories. We have showcased and plan to invite hospitalists with career expertise in high-value care, quality improvement, patient safety, clinical reasoning, hospital administration, advocacy, medical education, and more. Each Hospitalist shares their career path, highlighting pivotal moments along their journey and providing tips for developing a niche in a given area. One-hour informal sessions take place over Zoom.
 By George Hoke MD, Director of Faculty Development
By George Hoke MD, Director of Faculty Development
New Hospitalist Faculty Development
The Section of Hospital Medicine continues to grow and welcomed six new faculty members for the 2023 academic year. The transition from resident to faculty and from one institution to another can be quite complex. To help smooth this transition and ensure our new Hospitalists start their UVA careers on solid ground, Alex Millard and George Hoke have created an early career faculty development program. The components of this program include mentorship and a Professional Development Conference Series. Each participating Hospitalist is assigned a primary mentor from the Section of Hospital Medicine. This senior Hospitalist will serve as a guide for exploring the opportunities within Hospital Medicine at the University of Virginia. Additional mentors with expertise in the faculty member’s area of interest will be added to the mentorship team as needed. The mentorship team may include faculty from outside the Section of Hospital Medicine. After the first year, each faculty member will work with their mentorship team to create goals for year two. The Professional Development Conference Series kicked off in September with a session on Facilitating Safe and Effective Care Transitions led by Amber Inofuentes and Jess Dreicer. See the full schedule below. We believe this program will facilitate the development of clinical and nonclinical expertise in areas of personal interest to promote career satisfaction, faculty retention, and academic promotion.
September- Facilitating Safe and Effective Care Transitions
October – Documentation, and Billing
November – Effective Hand-off of care
January – Teaching ACE students on hospitalist rotations
February – Perioperative Medicine
March – Teaching the 3rd year student and resident team
April – Learner Evaluation and Feedback
May – Making the most of mentorship
 By Rahul Mehta MBBS, Director
By Rahul Mehta MBBS, Director
Perioperative and Consultative Medicine
To improve the perioperative skills of residents and post-clerkship students rotating on our elective, this year, we revamped the curriculum to one that focuses on the chronologic development of specific perioperative competencies during week one and week 2 of this rotation. We also improved preoperative risk stratification assessments to incorporate the latest evidence-based cardiovascular and pulmonary risk tools and added frailty and cognitive assessments. Our standardized preoperative consult note enables learners to systematically evaluate each important domain. To enhance faculty development and foster a collaborative learning environment with our Orthopedics NP colleagues, we also began a quarterly “Perioperative Case Conference”; sessions highlight a high-yield clinical case with a discussion of the latest practice-informing evidence. Cases presented this past year have featured topics ranging from neurogenic orthostatic hypotension to Ogilvie’s syndrome to preoperative risk assessment in cirrhosis.
RESEARCH HIGHLIGHTS
 By Omar Alsamman MD
By Omar Alsamman MD
Clinical Documentation Improvement Lead Physician
This year, the section will strengthen and expand its focus on improving clinical documentation in alignment with medical center and departmental priorities. Central to this work is creating a new leadership role for hospital medicine, the Clinical Documentation Improvement (CDI) Lead Physician, whose fundamental goal is to promote a positive environment for documentation. This role will serve as an important connector between the medical center, departmental coding staff, and frontline faculty and utilize a data-driven approach to improving our section’s clinical documentation at individual and group levels.
All new faculty (those in the first two years of practice) will participate in individual quarterly reviews, coaching sessions, and faculty development for the group, covering key themes and opportunities. The Lead Physician will also facilitate the implementation of AI tools (such as Regard, previously Health Tensor) designed to help physicians improve documentation accuracy, reduce time spent in the EMR, and partner with departmental data scientists to generate dashboards for continuous learning and improvement.
Given hospitalists’ unique role as both frontline clinicians and faculty supervising trainees, we are uniquely positioned to significantly impact the quality of clinical documentation; if successful, our documentation improvement program can serve as a model for other divisions and departments in future years.
QUALITY HIGHLIGHTS
 By Charles Magee MD, 3W Medical Director
By Charles Magee MD, 3W Medical Director
Cardiac Monitoring – Getting with the guidelines?
In late 2021, higher inpatient medicine volumes began to strain the hospital’s capacity for inpatient telemetry monitoring. On 3 West, our UBL (which I co-lead with nurse manager Scott Austin) noticed that general medicine and hospitalist team patients were placed on non-geographic units when no other telemetry slots were available on their home units. Initial investigation revealed a problem with telemetry overuse, a common quality problem in hospital settings. Using the “5 Whys” method, we identified root causes and opportunities for improvement. Starting with the simple question, “Does this patient need telemetry?” we identified knowledge gaps across the inter-professional care team resulting in a lack of standard practice for inpatient cardiac monitoring. With the assistance of performance improvement coach Evie Nicholson, our interdisciplinary team launched an effort to improve guideline-concordant telemetry usage and eliminate low-value telemetry days.
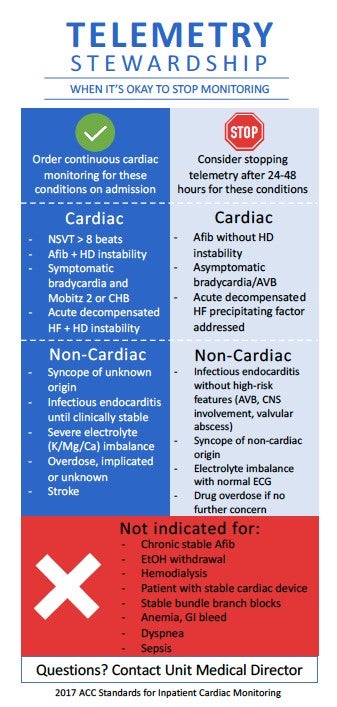 The first step of this process was a review of current literature and expert opinion; Dr. Magee and medicine resident Ford Franklin partnered with Dr. Pam Mason, Director of Electrophysiology Programs, to distill the 2017 American Heart Association guidelines for cardiac monitoring into a digestible format for frontline team members. The resultant simple infographic was used to educate physicians and nursing teams and alignment around guideline-informed cardiac telemetry stewardship. Telemetry stewardship was also added to daily interdisciplinary rounds (IDR), highlighted during weekly Quality Improvement rounds with house staff teams, and reviewed at weekly unit leader rounds to evaluate the initiative’s success and drive iterative improvements.
The first step of this process was a review of current literature and expert opinion; Dr. Magee and medicine resident Ford Franklin partnered with Dr. Pam Mason, Director of Electrophysiology Programs, to distill the 2017 American Heart Association guidelines for cardiac monitoring into a digestible format for frontline team members. The resultant simple infographic was used to educate physicians and nursing teams and alignment around guideline-informed cardiac telemetry stewardship. Telemetry stewardship was also added to daily interdisciplinary rounds (IDR), highlighted during weekly Quality Improvement rounds with house staff teams, and reviewed at weekly unit leader rounds to evaluate the initiative’s success and drive iterative improvements.
In February, Kelley Mark, a 4th-year medical student who selected the telemetry stewardship project for her quality improvement elective practicum, joined the unit in its effort. During her time, she conducted rigorous data collection demonstrating a 50% reduction in low-value telemetry utilization on 3 West compared to other acute care medicine units. Her data also confirmed the positive impact of interdisciplinary rounds by showing that most telemetry orders were discontinued in the hours following IDRs for geographic teams. Six months later, reductions in telemetry utilization and a palpable unit focus on telemetry stewardship persist. Patients are no longer geographically displaced due to a lack of telemetry monitoring capabilities.
To achieve sustainability and expand this successful work beyond 3 West, we are working toward modification of EMR telemetry orders to align with institutional guidelines, including indication-specific default durations. Additional stewardship opportunities include further investigation into telemetry order persistence following unit transitions within the hospital, as persistent orders from intensive care and post-procedural areas accounted for 43% of low-value telemetry orders. In summary, our interprofessional approach to quality improvement achieved the goal of reducing unnecessary cardiac monitoring, furthering our mission to always provide the proper care to the right patient every time.
Filed Under: Basic Research, Clinical Research, DOM in the News, Education, In the Know, News and Notes, Notable Achievements, Publications, Research, Top News
