Message from Pulmonary & Critical Care Division Chief, Imre Noth, MD

Imre Noth, MD
I am constantly awed and impressed by the dedication of the faculty within the Division of Pulmonary and Critical Care Medicine at the University of Virginia.
Over the last two years and entering a third now, the Division has faced the most difficult challenge in the COVID-19 pandemic over the last century. Yet, all the faculty has maintained an unbelievable level of professionalism and optimism towards the future through it. When the original shutdown took place in the spring of 2020, and people stayed home, we went to work in the ICU. While surges came and went, we found that our COVID ICU numbers never went down to zero. There was never a stoppage physical or emotional to the turmoil created by the pandemic. As of writing this message, we are in the peak portion of the omicron surge, and the sheer numbers are again reaching new heights. We have delivered the best possible care and a lower mortality rate than comparable institutions with the sickest patients. I’m not sure that we will ever be the same, but we are eager to move forward.
Amid all the chaos, we managed to keep building and expanding on three academic missions of excellence in patient care, education, and research. Since our last update, we now have 29 faculty members (six full Professors, nine Associate Professors, fourteen Assistant Professors). There are also over a dozen Nurse Practitioners and twelve clinical pulmonary and critical care fellows.
In our clinical programs, we have added several faculty just within the past year, with Subodh Pandey, MBBS, providing an additional trained Interventional Pulmonary specialist, greatly expanding our repertoire for patients with complex airways and minimally invasive techniques.
Charles Alex, MD, joined our transplant team over a year ago to help Drs. Mannem and Weder in the excellent care of our patients. Dr. Alex has three decades of experience in the Chicagoland area, as Chief of the Division at Loyola and Transplant Director at Loyola and Advocate Christ Hospital. Our homegrown Jamie MacLeod, MD, joined us this past year to further her work in COPD with Y. Michael Shim, MD. We also welcomed Katarine von Lang Egressy, MD, MPH, who has been instrumental in helping with our increased MICU numbers. Scott Schecter, MD joined us from the University of Iowa and has helped address our backlog in sleep medicine. Lastly, world-class immunologist Anne Sperling, PhD, joined us from the University of Chicago. We are excited at what she brings to our future research endeavors.
In our educational efforts, the faculty continue to garner teaching awards and applause from the medical students rotating through our services. Lastly, in the face of increasing our critical care output, the Division also concurrently increased its publication record over the last year, leveraging translational science resulting from the COVID-19 biorepository and the post-COVID clinic. Drs. Alexandra Kadl, Andrew Barros, and Jeffrey Sturek made notable contributions.
As we exit the darkness into the light, the future has never looked brighter for the Division, and I am excited to see where the next steps will lead us.
~ Imre Noth, MD, Division Chief
RESEARCH UPDATE
In 2021, the Pulmonary and Critical Care Division maintained and expanded a diverse research portfolio while considering pandemic clinical care’s rigors.
We are proud of our fellows, who have garnered research recognition and grants in biomedical engineering (Daisy Zhu, MD, Engineering Coulter Fellowship), sarcoidosis (Jimi Akingbade, MD, American Thoracic Society scholarship), and the iDRIV scholar’s program (Claire Debolt, MD, and Eva Otoupalova, MD).
Fellow Chintan Ramani, MD, and faculty Alexandra Kadl, MD, MS, forged new paths in clinical research on COVID-19 survivorship; publication of their experience caring for COVID-19 ICU survivors garnered national attention and has led to multi-center collaborations.
John S. Kim, MD, MS, received an NIH K23 award in 2021 to study the role of polyunsaturated fatty acids in pulmonary fibrosis and was recently lauded for his work modeling serum biomarkers of lung injury.
Andrew Barros, MD, MS, utilizes high dimensional electronic health record data and medical data science techniques to investigate hospitalization outcomes.
Jamie MacLeod, MD, studies the immunologic effects of calcineurin inhibition in lung transplants.
Jeffrey Sturek, MD, PhD, is an emerging leader in B-cell biology and received a new Ivy Foundation grant last year.
Catherine Bonham, MD, has a K23 to study T-cells in pulmonary fibrosis.
Drs. Kadl, Bonham, and Somerville, received Global Infectious Disease Institute funding for their COVID-19 immunophenotyping research and biorepository initiative.
Drs. Sturek, Kadl, Bonham, and Shim received Dean Kibbe’s 2022 Faculty Research Award for Team Science for their interdivisional initiatives on COVID-19.
Dr. Y. Michael Shim is continuously R01 funded for his work in COPD, using hyperpolarized Xenon-129 MRI to measure pulmonary physiologic responses to therapeutics.
Imre Noth, MD, holds R and U level funding in the study of idiopathic pulmonary fibrosis (IPF) genomics which he conducts with collaborators Shwu-Fan Ma, PhD, and Yong Huang, MD, MS.
Under Dr. Noth’s leadership, the University of Virginia is the lead site for the first-ever NIH-funded pharmacogenomics interventional trial in IPF (PRECISIONS).
In the area of transplant, Max Weder MD, Hannah Mannem MD, and Charles Alex, MD, blazed trails with one of the first COVID-19 lung transplants in the nation and launched an international database to track experiences and outcomes of COVID-19 lung transplant patients, who were the third leading indication for a lung transplant in 2021.
In the area of cystic fibrosis, Drs. Somerville and Albon innovated to deliver exceptional multidisciplinary telemedicine-based care, publishing their clinical research in CHEST. At the same time, cystic fibrosis respiratory therapist Martina H. Compton, RRT-NPS, RPFT received both the National Respiratory Patient Advocacy Award and the CF Foundation Outreach Award in 2021.
Finally, in 2021, we welcomed senior investigator Anne Sperling, PhD, whose internationally recognized expertise in translational immunology, asthma, pulmonary fibrosis, and mentorship in respiratory biology is truly an asset to the division and reflects our academic mission of excellence and scholarship.
INTERVENTIONAL PULMONARY
The Interventional Pulmonary sub-division of Pulmonary/Critical Care Medicine provides state-of-the-art care in minimally invasive pulmonary procedures. The multidisciplinary team works closely with other specialty departments of the Emily Couric Cancer Center, including Thoracic Surgery, Medical and Radiation Oncology, Pathology, Radiology, and Laryngology. Our team provides advanced diagnostic bronchoscopy, including endobronchial ultrasound, navigation bronchoscopy, and biopsy. We also offer a full array of therapeutic interventions in benign and malignant complex airway diseases, including tumor debridement and airway recanalization using rigid bronchoscopy, laser, argon, cryotherapy, ballon bronchoplasty, airway stenting, and thermoplasty. Our team also provides expertise in pleural disease management. We are excited to announce the addition of the ION robotic bronchoscopy platform and Endobronchial Lung Volume Reduction programs in the coming months.
SLEEP MEDICINE PROGRAM
In the past year, the sleep medicine program has added two new clinicians, Scott Schecter, MD, a Pulmonary/Critical Care Medicine/Sleep Medicine physician, who comes to us from the University of Iowa, and Matthew Burns, a newly minted NP, who comes to us from the UVA MICU. We currently have three physicians and two APPs, and two pediatric sleep clinicians in the program. UVA Health appears to be committed to the ongoing growth and development of the sleep medicine program, which is good because we continue to get referrals from across the state.
FELLOWSHIP PROGRAM UPDATE
RESEARCH WEEK
The 1st year PCCM fellows recently participated in their very own Research Week! The week was filled with presentations ranging from grant opportunities and research tracks to learning about the library and iTHRIV resources to faculty sharing their current research in a “speed dating” format. The fellows utilized these talks and the protected time to focus on deciding what type of research they would like to do as part of fellowship.
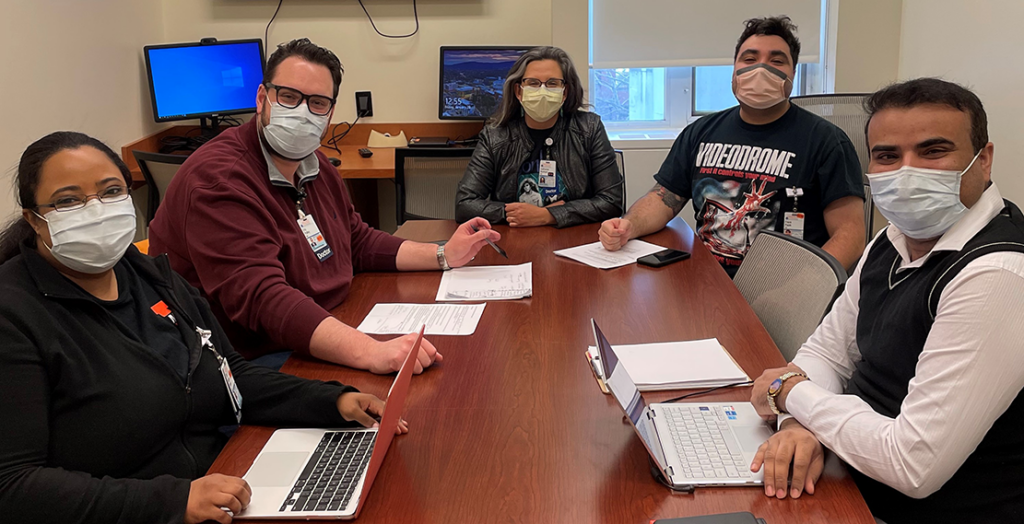
Dr. Catherine Bonham mentoring the first year fellows as they discuss their preliminary thoughts on potential research projects. Left to right: Dr. Naima Farah, Dr. Eric Polley, Dr. Catherine Bonham, Dr. Frank Papik, Dr. M. Ibrar Islam.
FELLOWSHIP PROGRAM UPDATE
The PCCM division started a quarterly “Procedural Skills Day” to help keep fellows and faculty skills sharp. They’ve focused on hands-on activities involving tasks ranging from advanced airway techniques to pumps & parts of extracorporeal membrane oxygenation (ECMO).

Fellows and faculty work to perform cricothyroidotomy on pig tracheas and intubate on the dummy.
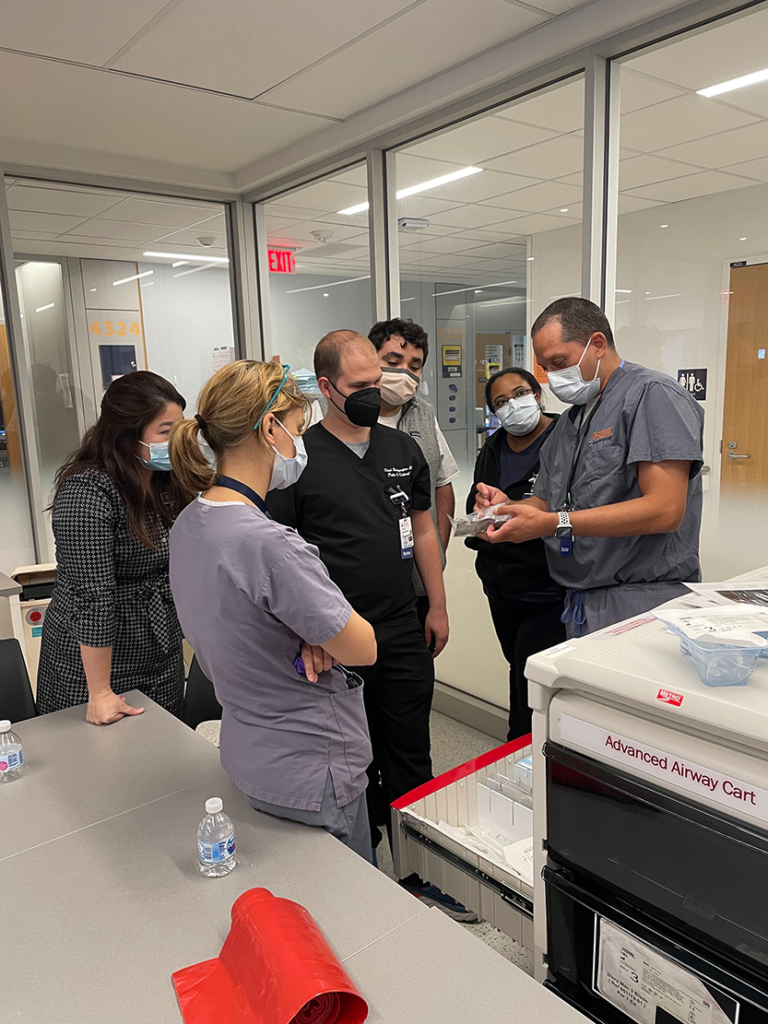
The team reviews the supplies available in an advanced airway cart with Dr. Andrew Barros.
PULMONARY EVENTS
COMMUNITY SERVICE – November 2021
 In 2019, there were 246,750 SNAP recipients in VA who were classified as elderly or disabled and the average food benefit for an older adult was $87 per a month or $0.81 per meal–some elderly persons receive the minimum benefit of only $16 per month or $0.15 per meal (www.cbpp.org).
In 2019, there were 246,750 SNAP recipients in VA who were classified as elderly or disabled and the average food benefit for an older adult was $87 per a month or $0.81 per meal–some elderly persons receive the minimum benefit of only $16 per month or $0.15 per meal (www.cbpp.org).
With these heartbreaking statistics in mind, the Division of Pulmonary and Critical Care partnered with the Greene County Department of Social Services (Stanardsville, VA) during November.
Our goal was to create gift bags filled with hygiene and comfort items to supplement twenty-five Thanksgiving food boxes.
Strictly by faculty and staff donations, we far exceeded that goal and could also made a cash donation of $250 to the Greene County foster children’s holiday gift fund.
Anne Winn, Greene County DSS Benefit Services Supervisor, accepted the gifts on behalf of the agency and was overwhelmed by the generosity of our team.
HOT COCOA FOR A CHILLY DAY – December 9, 2021
 The Division of Pulmonary and Critical Care hosted a hot cocoa bar in the Administrative area on December 9th. Faculty and staff were met with a lovely decorated bar that included an assortment of hot cocoa flavors, add-ons, and treats. Hot cocoa and fellowship were just what the doctor ordered on a chilly December day!
The Division of Pulmonary and Critical Care hosted a hot cocoa bar in the Administrative area on December 9th. Faculty and staff were met with a lovely decorated bar that included an assortment of hot cocoa flavors, add-ons, and treats. Hot cocoa and fellowship were just what the doctor ordered on a chilly December day!
CYSTIC FIBROSIS (CF) UPDATE
In response to the COVID-19 pandemic, three distinct models of interdisciplinary care have emerged from our UVA cystic fibrosis program. The standard of CF care delivery is a collaborative effort by a team of professionals with diverse areas of expertise. A typical CF care visit at UVA can often include between 5-7 care team member interactions per patient. In addition to the physician, these interactions may consist of a registered dietitian, respiratory therapist, clinical psychologist, social worker, and registered nurse coordinator.
The onset of the pandemic in March 2020 and its associated public safety mandates and recommendations set in motion a season of innovation and rapid adaptations by the CF team. The mission is to preserve their high standard of care while emphasizing patient and team safety, PPE conservation, and patient preferences.
Considering a matrix of variables like COVID positivity rates in the community, availability of objective health data, ability and willingness to utilize web-based health tools; patients with CF are triaged into one of three types of care visits personalized to their circumstances and preferences:
• Traditional: patient in person and team members in person
• Telehealth: patient and care team members connect virtually using Webex and utilize remote monitoring devices for spirometry and other patient-reported health data
• Hybrid: patient and physician are in person, and team members join the patient encounter via iPads placed in the exam room
Under the leadership of medical director Dr. Dana Albon, the CF care team has successfully preserved the critical components of the traditional CF care model and demonstrated agility and competence in adapting to the ever-changing landscape of the pandemic. This work has been shared nationally with peers in the CF Care Center Network and key pulmonary and telehealth journals. To learn more about the work being done by our CF team, please see publications in newsletter.
Filed Under: Basic Research, Clinical Research, Education, In the Know, News and Notes, Research
Tags: DOM, Education, faculty, March 2022, March 2022 Medicine Matters, March Medicine Matters, medicine matters, newsletter, profile, profiles, Publications, Pulmonary, Research, staff
