CLINICAL HIGHLIGHTS

Paul Helgerson, MD
By Paul Helgerson , MD, Vice-Chair for Inpatient Services and ACMO for Acute Care
Reflections on the Fifth (“Delta”) Wave
After a too-brief respite from high volumes of inpatient COVID care over the summer, the health system again finds itself rapidly adapting this fall to another surge. There was a bit of a deja-vu sensation for many of us as we recalled the emotions and lessons learned from March of 2020 and the early months of 2021 when the hospital saw its previous highs in admissions (and deaths) due to COVID-19. Equally striking, though, were the myriad ways in which our system and workforce had evolved. In the fall of 2021, we find ourselves with plenty of PPE but closely watching global supply chains for many other things we use daily (like suction canisters or fentanyl drips). We celebrate new therapeutic options but lament the uneven uptake of essential vaccines within our broader region. Most of all, we celebrate the talent of those who surround us but struggle day by day to maintain a stable interdisciplinary team that can expand to keep up with the demand based on local and national workforce turnover.
Division members have played a key role in partnering with others in the health system and community to meet the evolving challenges that the pandemic brings. Reflecting on these many contributions presents a microcosm of what the division, department, and our academic health system are about and gives me great hope for what we will accomplish together. Here are a few of the many remarkable ways in which you contribute to our collective job of “pandemic fighting.”
Compassion – My thanks to the many faculty, APPS, residents, and fellows who have taken on additional patient care duty to meet the needs of our COVID patients. Many have volunteered nights, weeks of coverage, or clinical assignments covering additional teams. It is more evident now than ever that we work among peers committed to patient care. You bring tremendous expertise to the bedside.
Adaptability – Where to start? New teams have started, stopped, moved, and rearranged. I am particularly grateful to our colleagues on non-general medicine teams and floors who recently admitted COVID-positive patients presenting with non-COVID primary diagnoses. These patients often have specialized needs and benefit from nurses and physician teams outside of the south tower. In addition, acute cardiology, trauma, orthopedics, OB/GYN, and many others have become accustomed to the workflows of COVID care to the benefit of both our patients and the busy 4S/5S teams.
Teamwork and Interdisciplinary Care – Our recent emphasis on structuring interdisciplinary rounds have been given a vital stress test in the last few months. As nursing ratios are stretched, turnover increases, and team members such as social work, case management, and respiratory therapy adjust to meet rising demand and short staff. I am profoundly thankful to the many colleagues working harder than ever. I am equally grateful to have a colleague like Peggy Plews-Ogan, who is a tireless advocate for the well-being of both our faculty and these essential partners.
Scholarship – In the past months, our general medicine teams have benefitted from the guidance of Patrick Jackson and Bill Petri as they introduce new treatment paradigms for our COVID patients. Most recently, many patients are opting to participate in the dupilumab trial, investigator-initiated at UVA. Thus, our patients are fortunate to receive care in an institution at the forefront of emerging COVID therapeutics and treatment protocols. It has also been a pleasure to see a partnership in clinical investigation grow within general medicine and to involve many of our new nursing staff in 5S in the effort.
Advocacy – On the first of October, we listened as our own Cameron Webb detailed the efforts the present administration is making to ensure efforts to vaccinate are equitable and robust. Locally, I’ve shared touching moments with expert clinicians like Mo Nadkarni and Amber Inofuentes as they have supported some of our highest utilizers through the trials and tribulations of vaccine hesitancy, a new COVID diagnosis, and ICU care.
Quality and Safety – Despite the shifting sands, we continue to find that our mortality in the population admitted with COVID is top-quartile within a group of peer academic medical centers. Despite headwinds related to staffing, fatigue, and volume, teams work daily to prevent hospital-acquired infections, implement new standards to ensure the best care, and evaluate new innovations.
I was once told that stress tends to exaggerate one’s most fundamental traits. In that light, I am not surprised to see these wonderful examples emerging as we meet the challenges that COVID has brought to our doorstep. Thanks for all you are doing.
By Amber Inofuentes, MD, Medical Director
Medicine HOME Program
The pandemic has presented many challenges to the care of vulnerable patients, including the frequently hospitalized patients enrolled in the Medicine HOME Program, which I direct in partnership with Clinical Program Coordinator Teresa Radford, RN. Though our program gained a full-time social worker in early 2020, this role was quickly redeployed to inpatient units to fill staffing shortages and meet the needs of surging inpatient volumes. This past September, the program moved under Population Health to consolidate resources to better meet patients’ social needs.
In early October, Guy Lushin, LCSW, rejoined our team full time. We manage an active census of 30-35 enrolled patients with a wide range of medical diagnoses and behavioral health challenges and have also begun to offer consultative services at the request of team members across the health system. This past summer, Dr. Ian Crane also joined the program as the physician lead for the Diabetes subgroup. This year, we will be piloting a ‘bridge’ clinic for a small number of enrolled patients to provide home-based primary care and plan to publish the results of a qualitative study highlighting barriers to care from the perspective of enrolled patients.
COMMUNITY HIGHLIGHT
Hospitalists Sponsor Afghan Refugee Family through IRC
Working through the International Rescue Committee (IRC), members of the Section of Hospital Medicine sponsored a refugee family from Afghanistan who immigrated to Charlottesville in May of this year. Jess Dreicer, Miriam Gomez-Sanchez, Meghan Geraghty, Andrew Parsons, and George Hoke, joined by their spouses/families, formed a HOME (Housing, Outreach, Mentorship, Education) team to assist the family of three in a challenging transition to a new life in a new country. Before their arrival, our team was trained by IRC staff in how to assist refugees. We then set up an apartment for the family, supplying furniture, kitchen supplies, household goods, and stocking the refrigerator and pantry. We also contributed $3000 in rental assistance. On May 6th, we met mom, 18-year-old daughter, and 14-year-old son at the Charlottesville airport and welcomed them to Charlottesville. Since then, we have assisted them in shopping outings, dropped off pizza for dinner (the kids’ favorite), dropped off excess vegetables from our gardens (mom’s favorite). More recently, we have started to teach the 18-year-old daughter to drive. She is the first person in her entire family ever to drive a car. Mom is working at the Omni hotel and taking English classes at the Jefferson School. The son is thriving at Buford Middle School and is hoping to play soccer. Overall they are doing quite well. We hope to get to know them better as they acclimate to a new life and COVID concerns wane.
RESEARCH HIGHLIGHTS

Shrirang Gadrey, MD
By Shrirang M. Gadrey, MBBS MPH
Analysis of Respiratory Kinematics (ARK): novel respiratory monitoring technology developed at UVA
An essential duty of a hospitalist is to detect the earliest signs of clinical deterioration. My experiences as a hospitalist taught me that inspection of breathing motion patterns helps with the early detection of imminent respiratory decline. Normal breathing appears regular, effortless, well-coordinated, and comfortable. However, many kinds of abnormal breathing patterns can be seen in patients at high risk of respiratory deterioration. Labored breathing, for example, is a significant red flag sign – it signifies respiratory muscle overload that can progress to fatigue. Similarly, the emergence of irregular (“ataxic”) breathing in response to narcotic pain medicines is an early warning sign of an imminent overdose.
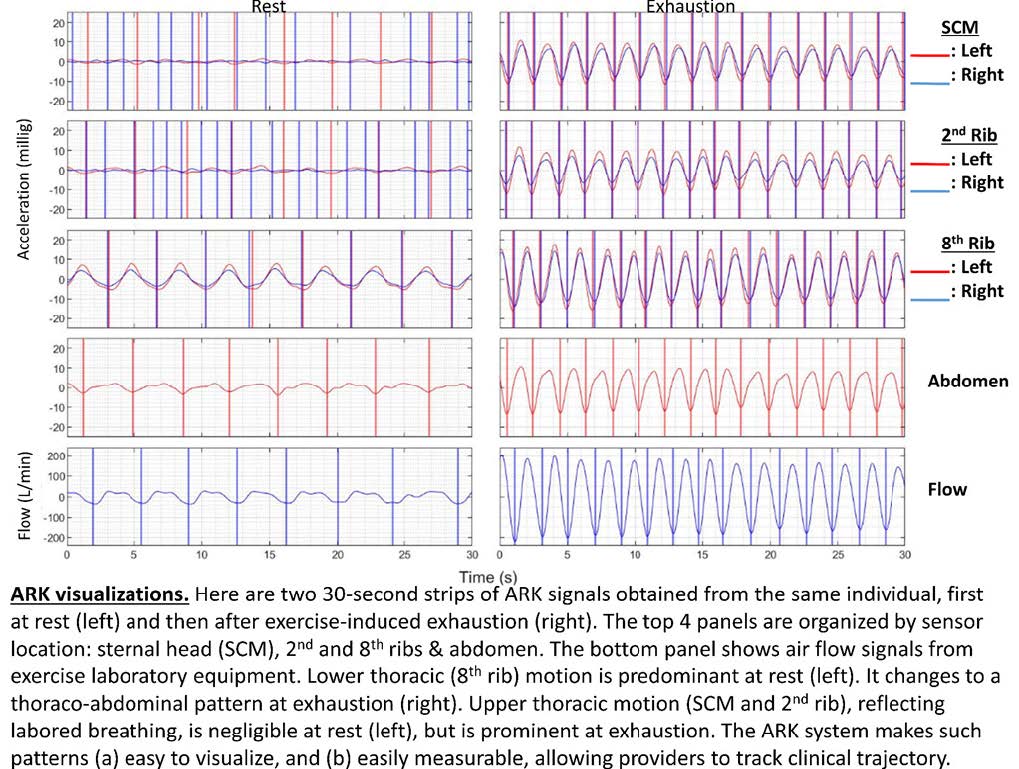
It became increasingly clear that breathing motion patterns are essentially a distinct family of “vital signs,” conveying crucial diagnostic and prognostic information not conveyed by other vital signs. For example, when evaluating a patient with pneumonia and labored breathing, my clinical acumen suggested a high risk of deterioration, even if vitals like the respiratory rate were documented as normal (often erroneously!). So I asked myself the simple questions: Why isn’t breathing motion characterized quantitatively and researched rigorously like every other vital sign? Why must I describe my findings in adjectives and phrases rather than numbers that can be used in predictive modeling? These questions inspired me to develop the “Analysis of Respiratory Kinematics (ARK)” method for quantitative characterization of breaths. The results of my work to date are highly encouraging. They are shown in the figure below, and a pre-print is available at: https://www.medrxiv.org/content/10.1101/2021.09.06.21263179v1.full-text.
An analogy with blood pressure measurement methods helps convey the potential impact of the ARK method. Before the invention of sphygmomanometers, clinicians assessed blood pressure qualitatively based on the manual compressibility of the pulse. After blood pressure became readily measurable at the bedside, its enormous diagnostic and prognostic power was fully harnessed, and entirely new pathophysiologic insights were uncovered. With the ARK system, I aim to make respiratory kinematics readily measurable at the bedside. This can unlock a new area of research and enhance patient safety. My vision is that the ARK system will lead to easier, earlier, and better diagnosis of abnormal breathing motion, helping busy clinicians quickly identify patients at highest risk of imminent respiratory collapse.
EDUCATION HIGHLIGHTS

Andrew Parsons, MD
Innovative Education in Quality Improvement
Bahnsen Miller, MD, Charlie Magee, MD, and Joe Hall, MD conduct weekly ‘QI Rounds’ to engage residents and students in unit-based quality improvement and patient safety initiatives. Recent examples include team-based case management, overnight plan of care notes, and improved utilization of Vocera communication devices. George Hoke, MD and Paul Helgerson, MD have led efforts to simplify and standardize daily interdisciplinary rounds. A short video was created to educate care teams on making rounds more efficient and effective for patient care. Finally, Andrew Parsons, MD, and Amber Inofuentes, MD, designed and implemented a curriculum for IM and SAGO clerkship students utilizing novel QI & Patient Safety and High-Value Care “workouts” paired with faculty-led discussions.
Remediation of Struggling Learners
Several hospitalists continue to make contributions to the GME and UME remediation programs. Greg Young, MD, Andrew Parsons, MD, and Jess Dreicer, MD, conduct one-on-one sessions focused on clinical reasoning as part of COACH, the GME-wide remediation program. Many others have hosted residents on clinical rotations for focused teaching and assessment. George Hoke, MD leads the Mastery Elective, an inpatient clinical rotation composed of intense one-on-one clinical performance development for students in need of remediation based on EPA data. Finally, Ian Crane, MD and Greg Young, MD serve as specialty coaches for the UME clinical remediation program, designing evidence-based resources and conducting individualized sessions for select students as part of a multidisciplinary team.
Foundations of Clinical Medicine
Launched in 2018, the Foundations of Clinical Medicine (FCM) program is a novel (https://pubmed.ncbi.nlm.nih.gov/32804347) 4-year long curriculum focused on clinical skill development and professional identity formation. The program has had continued success and consistently strong hospitalist involvement. Within the UVA School of Medicine curriculum, morning lectures concern themselves primarily with basic science knowledge. The practice of medicine—both the science and the art in all of its subtleties – is the focus of FCM. Despite continued constraints imposed by the COVID-19 pandemic, the FCM program has had another successful year! This success is due, in large part, to the hospitalists who serve as physician coaches: Becky Kenner, MD; Ben Sneed, MD; Chris Moore, MD; Rahul Mehta, MD; Glenn Moulder, MD; Greg Young, MD; Usmaan Bashir, MD; and Andrew Parsons, MD who directs the FCM Program. Charlie Magee, MD; Alex Lawson, MD; Ian Crane, MD; David Fink, MD; and Ryan Wiggins, MD serve as substitute coaches.
Intersessions Course
The Intersessions Course began in March 2021 and is co-directed by Dr. Greg Young. This multidisciplinary course is comprised of three one-week sessions paired with each trimester of a student’s clerkship year. The threefold main goals objectives of the course are for students to (1) integrate learning experiences to enhance clinical learning through activities designed to revisit basic science, incorporate curricular threads, and practice clinical skills such as physical exam techniques, diagnostic reasoning, quality improvement, communication, and other clerkship-specific procedures and skills; (2) explore and expand personal career interests with exposure to areas of clinical medicine not currently included in the clerkship year; and (3) meet with their Foundations of Clinical Medicine (FCM) coaches to review clinical performance data and create individualized learning plans.
UVA Hospital Medicine Grand Rounds
Hospital Medicine as a national specialty, specifically at UVA, fills an important niche within the internal medicine community. To address hospitalists’ specific faculty development needs, we recently kicked off “UVA Hospital Medicine Grand Rounds.” This monthly series hosts expert speakers on various topics specific to inpatient medicine and provides Category 1 CME. All are welcome!! Speakers to date have included internal experts in Behavioral Medicine (Dr. Joey Yost) and Diabetes (Dr. Jen Kirby) as well as external experts in Point of Care Ultrasound (Dr. Carrie Herzke, Johns Hopkins University). Stay tuned for upcoming speakers this year!
Filed Under: Basic Research, Clinical Research, Education, Research
