Nationally, we are observing that many major medical centers are using service lines to manage their clinical operations. The American Association of Medical College’s Advisory Panel on Health Care has recommended service lines as a best practice for providing “integrated, high quality, patient centered care with efficiencies gained from reducing/duplicative administrative cost and from centralizing support functions”. 1
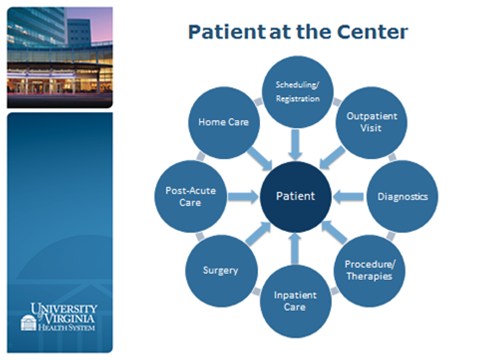
The patient is at the center of the story and the service line is the path in which they will travel.
Our Cancer Center already operates in the management model of a service line. When a patient is referred for a suspicious mammogram, for example, multiple distinct disciplines engage with each other to coordinate her care – from radiology and pathology to surgical and radiation oncology. LIPs from different disciplines are involved. Because of geographic proximity, interdisciplinary discussions ensue for a plan of care. Of course, there are many others who may be involved in this patient’s care – respiratory therapists, physical therapists, occupational therapists, nutrition services, etc. This happens at the Emily Couric Cancer Center, although there might be an admission to the 8th floor for concerns or complications as they arise.
These providers, all who work with cancer patients, may have more in common with each other than with members within their own Departments. This is the premise of the service line – to link groups which are connected by the patient or disease, and their spaces, to each other. The providers in the Cancer Center know each other, and use protocols and best practices to inform decision making. They share resources, and harness each other’s ideas to grow. They belong to departments, but work within a service line.
We envision eleven services lines at the University of Virginia with some support lines (such as Radiology, Laboratory Medicine and Pathology). Each service line will have a lead physician (or 2 physicians co-leading) and an administrative lead from the Medical Center (a manager or a director). These leads will be dyads (physician/administrator) with collaborative decision making (resource allocation, sharing and growth).
You might ask yourself how this might impact you. For some of you, it will feel no different. You will still be in a School of Medicine Department, and you will report to a Chair. You may already be in a service line. For others, you will remain in your Department, but your Department will now work with one or a number of service lines (for example, you work exclusively with one population – such as neuro-oncologists do). However, for everyone, there will be more resources to share and an ability to grow.
We are really looking forward to building up these service line teams and to focusing all of our resources on patient centered care. – cg
- Enders T, Conroy J. Advancing the Academic Health System for the Future. A Report from the AAMC Advisory Panel on Health Care. American Association of Medical Colleges. Available at www.aamc.org/download/370550/data/advancing.pdf
(Thanks to Posy Marzani and Jack Jackson for their help with this blog).
Filed Under: Integration, Service Line

Comments