The term “population health” is over a decade old now, but still relatively new in the public consciousness. It has been defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group” (Kindig, D. & Stoddart , G. “What is Population Health”. Am J Public Health. 2003 March; 93(3): 380–383. The goal is to improve the overall health of the population. A conceptual outcome of this is the Accountable Care Organization or ACO.
Well Virginia is a Medicare Shared Savings Program Accountable Care Organization. What this means, for us, is that anyone who is insured under Medicare Fee for Service (FFS) and is identified as a UVA patient—for primary care purposes – one who is either associated with a primary care provider at UVA or who receives the bulk of their Evaluation and Management services at UVA (and does not have an identified PCP) — qualifies. We must meet 33 quality metrics, which are tracked from year to year. If we meet these and quality metrics, and if we achieve a minimum savings rate (2.5%), then we will qualify to receive (“share”) 1/2 of the money saved (“savings”) from CMS (the Center for Medicare and Medicaid Services). Over 20, 000 Medicare FFS beneficiaries are attributed to this ACO. 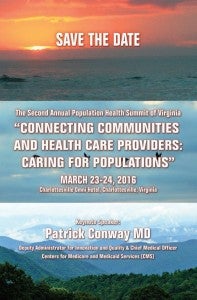
Daniel McCarter, M.D., the Medical Director for Well Virginia, (our ACO) feels that the explanation that Dr. Rick Shannon uses is hard to beat: “Provide the right care to the right patient in the right location, the first time, every time, without error, defect, or waste”.
CG: “What is the basic goal of the program?”
McCarter: “When talking about population health we hear about Don Berwick’s (or the Institute for Healthcare Improvement’s) triple aim—improving the health of the overall population, while reducing the cost of care for that care and improving the patient experience. However, it is important to add a 4th Aim to this process—we have to maintain or improve the healthcare professionals’ and staffs’ experience as well. They come to work every day because at some point they decided that they wanted to make people’s lives better. We have to understand that and work to help them achieve the fulfillment that brought them to the caring professions to begin with. In addition to help making patients’ lives better we have to work to make their care providers’ lives better”.
CG: “What are the major barriers to implementing population health here? What about healthcare providers themselves?”
McCarter: “One of the unique issues that we are dealing with when moving from fee for service to value based healthcare or population health is how to do we engage the health care team, the community, the patient’s family and the patient to provide care in the “in between times”– Between office visits, between being discharged from the hospital and when they follow up again etc. It is about how to care for the patient at times when they are not right in front of the providers”.
Rajesh Balkrishnan, Ph.D., Professor of Public Health Sciences in the School of Medicine is the Co-Program Director of the Population Health and Prevention Research at the University of Virginia.
According to Balkrishnan, this program: “fulfills a strategic mission of the UVA School of Medicine through team-science led research and educational activities related to the social determinants of health and disease in diverse populations both nationally and internationally. Faculty are involved in research examining issues of effectiveness, efficiency and equity in the access, provision and outcomes of health care services for major illness and health conditions across the continuum of prevention. The Program’s educational and outreach programs are focused on translating research advances in the determinants of health disparities through the application of social science methods to evaluate health care programs and interventions and inform health care policy and decision making.”
CG: “What are the major barriers to population health?”
Balkrishnan: “In our research we have shown that major barriers include but are not limited to access to appropriate medical care, lack of awareness and education related to available treatment and prevention options, inefficient use of health care resources and finally health care treatments which are not truly effective in the real world.”
CG: “How do you see these contributions or efforts translating into patient care?”
Balkrishnan: “We believe by understanding how treatments and medical care policies and interventions work in different populations and what could be done to optimize their effectiveness, we will ultimately improve patient care by demonstrating value of truly effective treatments. Our approach of using real world patient data and working with both systems and communities to optimize prevention and treatment-related decision making for all stakeholders will ultimately translate to better patient outcomes and a healthier society.”
CG: “How does this impact healthcare providers?”
Balkrishnan: “Healthcare providers are actively seeking solutions as well as we move into an era of patient-centered medicine. We understand that populations are living longer lives but are battling chronic disease and related disability. Providers are definitely interested in making health care more patient friendly and are looking for solutions in which they can make patient decision making related to self care optimal for the best patient outcomes. Thus our research aids healthcare providers also to target patients who may be in most need of targeted and/or tailored health care interventions.”
So, you can see we are attending to these issues on multiple fronts. You are likely to see or already see patients who are part of Well Virginia. For more information, including on our public reporting and links to some FAQs, please go to: http://www.wellvirginiaaco.com/. Also, details on our Second Population Health Summit is below. – cg
Filed Under: ACO, Education, Integration, Population Health

